Excretory System is an important topic in Biology that deals with the process of removing waste materials from the body to maintain a healthy internal environment. It involves specialized organs like the kidneys, lungs, skin, and liver, which work together to eliminate metabolic wastes and regulate water and salt balance.
Excretory system
Excretion and Nitrogenous Waste Management in Animals
- Animals produce various metabolic and ingested by-products, including ammonia, urea, uric acid, carbon dioxide, water, and ions such as Na⁺, K⁺, Cl⁻, phosphate, and sulfate.
- These substances must be eliminated to maintain homeostasis. The type of nitrogenous waste and the mechanism of its excretion depend on the animal’s habitat and evolutionary adaptations.
Types of Nitrogenous Wastes:
- Ammonia:
- Toxicity: Ammonia is the most toxic form of nitrogenous waste.
- Water Requirement: Its elimination requires large amounts of water.
- Excretion Process: Ammonia is highly soluble and is excreted by diffusion through body surfaces or gills as ammonium ions (NH₄⁺).
- Organ Involvement: Kidneys do not play a significant role in ammonia excretion.
- Examples of Ammonotelic Animals: Many bony fishes, aquatic amphibians, and aquatic insects excrete ammonia directly and are classified as ammonotelic.
- Urea:
- Toxicity: Less toxic compared to ammonia.
- Water Requirement: Requires less water for excretion than ammonia, making it suitable for terrestrial animals.
- Excretion Process: Ammonia is converted into urea in the liver via the urea cycle (ornithine cycle). Urea is then transported through the blood to the kidneys, where it is filtered and excreted.
- Adaptations: In some animals, a small amount of urea is retained in the kidney matrix to maintain osmolarity.
- Examples of Ureotelic Animals: Mammals, terrestrial amphibians, and marine fishes excrete urea and are called ureotelic.
- Uric Acid:
- Toxicity: Uric acid is the least toxic form of nitrogenous waste.
- Water Requirement: Excreted with minimal water loss, making it highly suitable for water conservation in arid environments.
- Excretion Process: Uric acid is excreted as a paste or solid pellet, minimizing water loss.
- Examples of Uricotelic Animals: Reptiles, birds, land snails, and insects excrete uric acid and are termed uricotelic.
The Human Excretory System:
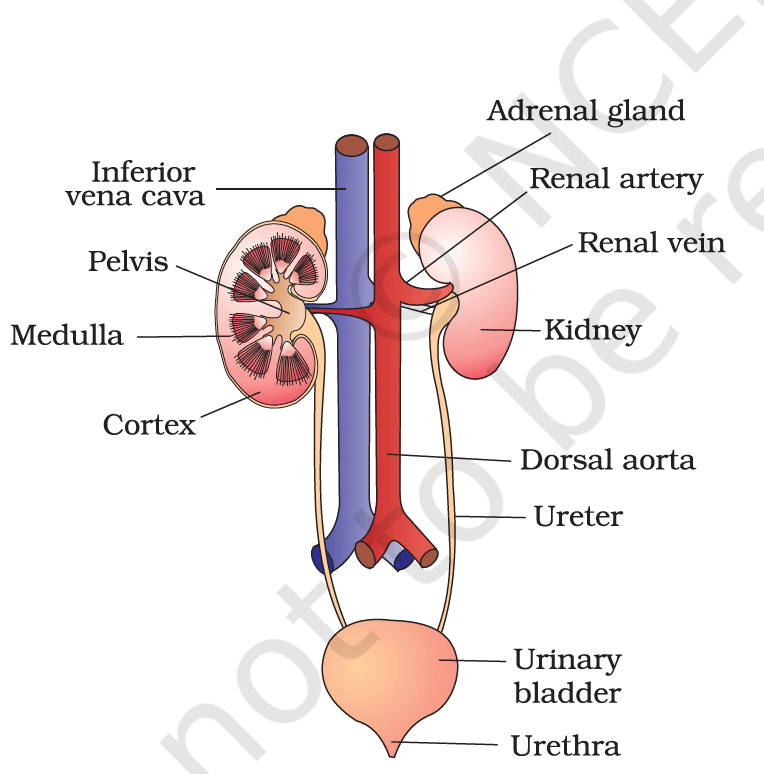
Fig: Human Urinary system
- The human excretory system is responsible for the removal of nitrogenous wastes and the maintenance of fluid and electrolyte balance in the body.
Main Components:
- Kidneys: Primary organs of excretion. The kidney house the structural and functional unit called the nephron, which performs filtration and urine formation.
- Ureters: Tubes that carry urine from the kidneys to the bladder.
- Urinary Bladder: Stores urine until excretion.
- Urethra: Transports urine from the bladder to the outside.
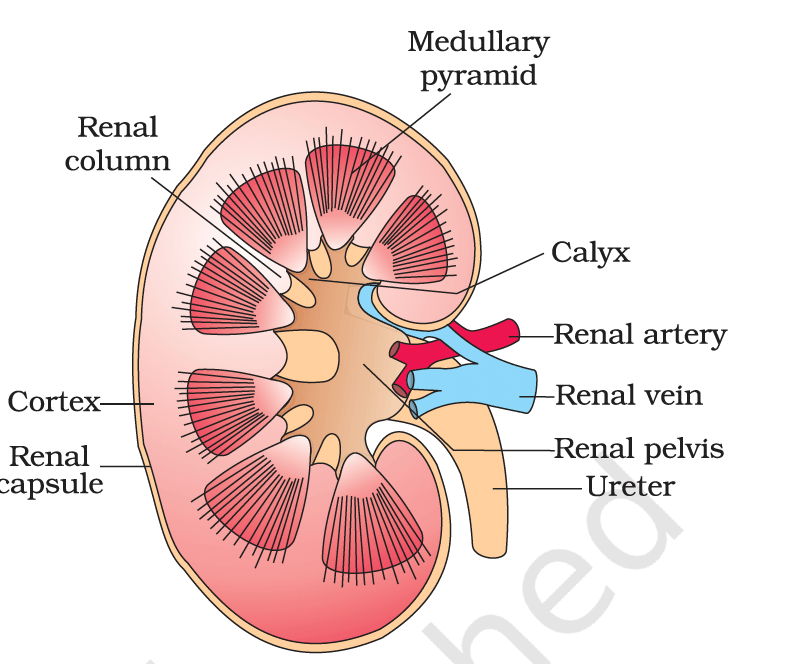
Kidneys:
- Structure: The kidneys are two reddish-brown, bean-shaped organs located on either side of the vertebral column, between the last thoracic and third lumbar vertebrae.
- Each kidney measures about 10-12 cm in length, 5-7 cm in width, and 2-3 cm in thickness, with an average weight of 120-170 grams.
- Inside the kidney, a renal pelvis with projections called calyces collects urine and directs it to the ureter.
- Zones:
- Outer Cortex: The peripheral layer of the kidney.
- Inner Medulla: The inner region.
The Nephron
The nephron is the functional unit of the kidney, responsible for forming urine through filtration, reabsorption, and secretion. Each kidney contains around one million nephrons, and every nephron has two main parts:
1. Malpighian Corpuscle (Renal Corpuscle)
This is the site of filtration and consists of:
- Bowman’s Capsule: A cup-shaped structure that surrounds the glomerulus and collects the filtrate.
- Glomerulus: A cluster of tiny blood capillaries where blood is filtered. Blood enters via the afferent arterioleand exits through the efferent arteriole.
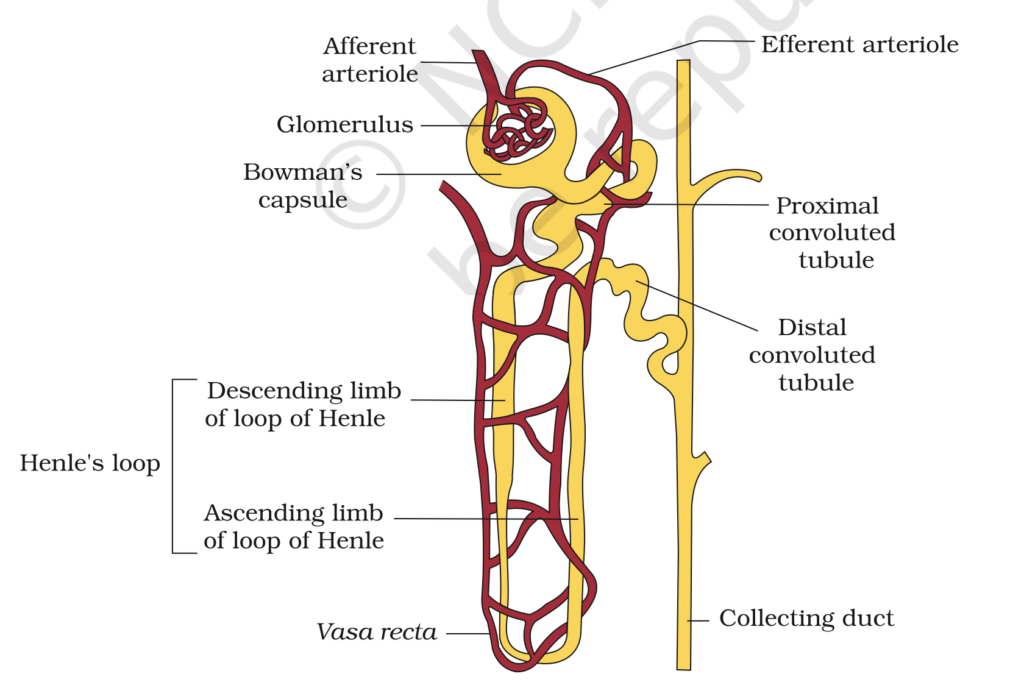
2. Renal Tubule
This is a long, tubular structure that modifies the filtrate into urine. It has four main parts:
a) Proximal Convoluted Tubule (PCT)
- Structure: A coiled tube located in the kidney’s cortex.
- Function: Reabsorbs essential nutrients (like glucose and amino acids), ions, and water from the filtrate.
b) Henle’s Loop
- Structure: U-shaped with a descending limb (goes down into the medulla) and an ascending limb (comes back up).
- Function:
- Descending limb: Reabsorbs water.
- Ascending limb: Transports ions but does not allow water reabsorption, creating a concentration gradient in the kidney.
c) Distal Convoluted Tubule (DCT)
- Structure: Coiled and located in the cortex.
- Function: Regulates ion exchange (like sodium and potassium) and helps balance pH levels.
d) Collecting Duct
- Structure: A straight tube where many DCTs connect. It drains into the renal pelvis.
- Function: Concentrates urine under the control of hormones like antidiuretic hormone (ADH).
Blood Supply to the Nephron
- Afferent Arteriole: Brings blood to the glomerulus for filtration.
- Efferent Arteriole: Carries filtered blood away and forms peritubular capillaries that surround the tubules.
- Vasa Recta: A U-shaped blood vessel in juxta-medullary nephrons that aids in maintaining the kidney’s concentration gradient.
Types of Nephrons
- Cortical Nephrons
- Short Henle’s loop.
- Located in the cortex.
- Less or no vasa recta.
- Juxta-Medullary Nephrons
- Long Henle’s loop extending into the medulla.
- Well-developed vasa recta.
- Helps produce concentrated urine.
Ureters
- Structure: Each kidney is connected to the urinary bladder by a thin, muscular tube called the ureter.
- Function: Transports urine from the renal pelvis to the bladder through peristaltic movements.
Urinary Bladder
- Structure: A muscular, hollow sac located in the pelvic cavity.
- Function: Temporarily stores urine. The bladder’s walls have stretch receptors that trigger the urge to urinate.
Urethra
- Structure: A tube that connects the bladder to the outside of the body.
- Function: Expels urine during the process of micturition. In males, it also serves as a passage for semen.
Urine Formation in Humans
The process of urine formation removes wastes like urea, excess salts, and water while balancing electrolytes, pH, and body fluids. It occurs in the nephron through three main steps:
1. Glomerular Filtration (Ultrafiltration)
- What Happens?
Blood is filtered in the glomerulus (a capillary network) inside the Bowman’s capsule. This step filters water, salts, glucose, and waste (like urea) but prevents large proteins and blood cells from passing through. - Mechanism:
- Blood enters via the afferent arteriole (wider) and exits through the efferent arteriole (narrower), creating high pressure for filtration.
- The filtrate passes through three layers.
- Result:
The filtered liquid, called glomerular filtrate, contains water, salts, glucose, and wastes. - Key Term: GFR (Glomerular Filtration Rate)
- Definition: The volume of filtrate formed per minute (~125 ml/min or 180 liters/day in healthy adults).
- Regulation: Controlled by the Juxta-Glomerular Apparatus (JGA).
2. Tubular Reabsorption
- What Happens?
Nearly 99% of the filtrate is reabsorbed back into the blood to retain essential nutrients, water, and ions. This happens in the renal tubule through active transport (requires energy) and passive transport (diffusion).
a) Proximal Convoluted Tubule (PCT):
- Role: Reabsorbs the majority of:
- Nutrients: Glucose and amino acids.
- Ions: Sodium (Na⁺), Chloride (Cl⁻), Bicarbonate (HCO₃⁻).
- Water: Via osmosis.
- Maintains pH:
- Secretes H⁺ ions and ammonia (NH₃) into the filtrate.
- Reabsorbs HCO₃⁻ to buffer blood pH.
b) Henle’s Loop:
- Role: Maintains a concentration gradient in the kidney’s medulla through the countercurrent mechanism.
- Descending Limb:
- Permeable to water (water exits into medulla).
- Concentrates the filtrate.
- Ascending Limb:
- Permeable to salts (actively pumps Na⁺, Cl⁻, and K⁺ into the medulla).
- Dilutes the filtrate.
- Descending Limb:
c) Distal Convoluted Tubule (DCT):
- Role: Reabsorbs water and Na⁺ under hormonal control (e.g., aldosterone).
- Maintains pH:
- Secretes H⁺, K⁺, and NH₃.
- Reabsorbs bicarbonate (HCO₃⁻).
d) Collecting Duct:
- Role: Reabsorbs water under the control of antidiuretic hormone (ADH).
- Concentration: Concentrates urine as it passes through the hyperosmotic medulla.
- Transports urine to the renal pelvis.
3. Tubular Secretion
- What Happens?
The nephron actively secretes additional substances into the renal tubule from surrounding capillaries. - Substances Secreted:
- Hydrogen ions (H⁺): Regulate blood pH.
- Potassium ions (K⁺): Maintain ionic balance.
- Ammonia (NH₃): Detoxifies nitrogen waste.
- Function:
- Eliminates drugs, toxins, and wastes.
- Maintains blood pH and electrolyte levels.
Summary of Urine Formation Process
- Glomerular Filtration: Blood filtration in the glomerulus forms the primary filtrate.
- Tubular Reabsorption: Recovery of essential substances and water from the filtrate.
- Tubular Secretion: Removal of additional wastes and maintenance of ionic/pH balance.
The final product—urine—is excreted through the ureters to the bladder.
Volume and Composition of Final Urine
- Daily urine output: 1.5 liters (on average).
- Composition:
- Water (~95%).
- Nitrogenous wastes (urea, uric acid, creatinine).
Regulation of Kidney Function
The kidney’s functioning is regulated by hormonal feedback mechanisms involving the hypothalamus, the juxtaglomerular apparatus (JGA), and, to some extent, the heart.
1. Osmoregulatory Mechanisms
- What Happens?
- When your body loses water, special sensors (osmoreceptors) detect it.
- The hypothalamus signals the release of antidiuretic hormone (ADH) from the pituitary gland.
- ADH’s Role:
- Saves Water: Makes the collecting ducts absorb more water back into the blood, reducing urine.
- Increases Pressure: Narrows blood vessels, raising blood pressure and boosting kidney filtration.
2. Renin-Angiotensin-Aldosterone System (RAAS)
- Why It Kicks In?
- If blood flow or pressure to the kidney drops (e.g., dehydration or low blood pressure).
- What It Does:
- The kidney’s JGA releases renin, starting a chain reaction.
- Renin turns a liver protein into angiotensin II, which:
- Tightens Blood Vessels to raise pressure.
- Triggers the hormone aldosterone, which helps kidneys reabsorb salt (Na⁺) and water, increasing pressure and fluid levels.
3. Atrial Natriuretic Factor (ANF)
- When It Helps:
- If blood pressure is too high, the heart releases ANF.
- What It Does:
- Relaxes Blood Vessels: Lowers pressure.
- Counters RAAS: Prevents too much salt and water reabsorption.
Micturition
- Definition: The process of releasing urine from the bladder through the urethra is termed micturition. It is governed by a micturition reflex.
Steps:
- Storage:
- Urine from the kidneys is stored in the bladder. (nephrons → ureters → bladder).
- When the bladder fills, it stretches, triggering sensors.
- Release:
- The brain gets the signal and sends a message to the bladder.
- The bladder contracts, and the urethral sphincter relaxes to release urine.
- Urine Characteristics:
- Light yellow, slightly acidic (pH ~6.0).
- Contains: Urea, NaCl, water, etc.
- Daily excretion : 1-1.5 liters.
Hemodialysis and Kidney Transplantation
Hemodialysis:
- Hemodialysis is a treatment for uremic patients with kidney failure where the machine filters waste from the blood.
How it works:
- Blood is drawn from a vein and passed through an artificial kidney (dialyzer).
- The dialyzer removes waste like urea and excess salts, using a special membrane and fluid.
- Clean blood is then returned to the body. (with anticoagulants to prevent clotting).
- This process provides temporary relief for kidney failure patients.
Kidney Transplantation:
A kidney transplant involves replacing a failing kidney with a healthy one from a donor. → Ultimate treatment for patients with acute renal failure or end-stage kidney disease.
- The donor kidney is usually from a close relative to reduce rejection risks. The new kidney restores normal function, eliminating the need for dialysis. Immunosuppressive drugs are used to prevent rejection.
Renal Disorders
1. Renal Calculi (Kidney Stones):
Kidney stones are solid crystals made of salts and minerals like calcium and uric acid that form in the kidneys.
Effects:
- Cause pain if they block the urinary tract.
- May lead to kidney swelling (hydronephrosis) or urinary tract infections (UTIs).
Treatment:
- Drink more fluids, use medications, or have surgery/lithotripsy to break or remove stones.
2. Glomerulonephritis:
Inflammation of the glomeruli in the kidneys, often caused by infections or autoimmune diseases.
Symptoms:
- Blood or protein in the urine and swelling.
- Can lead to chronic kidney disease or kidney failure if untreated
Treatment:
- Treat underlying causes like infections (antibiotics) or autoimmune issues (immunosuppressants).
Disorders of the Excretory System
- Uremia: Build-up of urea in the blood due to kidney failure.
- Symptoms: Fatigue, nausea, confusion, and urine-like breath odor.
- Treatment: Hemodialysis or kidney transplant.
- Hemodialysis: A process that filters blood using a dialyzer when kidneys fail.
- Procedure: Blood is drawn, cleaned in the dialyzer, and returned to the body.
- Other Conditions:
- Glycosuria: Glucose in urine, often from diabetes.
- Ketonuria: Ketones in urine, linked to diabetes or starvation.
Role of Other Organs in Excretion
In addition to the kidneys, the lungs, liver, skin, and even salivary glands contribute to waste elimination.
1. Lungs:
- Eliminate CO₂ (~200 mL/min) and water vapor during exhalation.
2. Liver:
- Metabolizes harmful substances and secretes bile pigments (e.g., bilirubin, biliverdin), cholesterol, and degraded hormones, which are excreted with feces.
3. Skin:
- Sweat glands:
- Excrete NaCl, small amounts of urea, and lactic acid.
- Primary role: Thermoregulation via evaporative cooling.
- Sebaceous glands:
- Secrete sebum, which contains lipids like sterols and hydrocarbons, offering protection for the skin.
4. Saliva:
- Contains small amounts of nitrogenous waste, contributing minimally to excretion.
