Blood groups Composition and Functions of blood are important topics in Biology that help us understand the vital role blood plays in our body. Blood is a special connective tissue that transports oxygen, nutrients, and hormones while removing waste products. It is classified into different blood groups and is made up of plasma, red blood cells, white blood cells, and platelets, each performing essential functions for survival.
Previous year Questions
| Year | Question | Marks |
| 2018 | What is the role of Haemoglobin in Human blood ? | 2M |
| 2016 | Explain the inheritance of ABO blood groups in human beings. | 5M |
| 2016 | What are monoclonal antibodies ? How are they produced ? | 10M |
| 2013 | What is Blood Pressure ? What is the normal range of blood pressure and which is the instrument is used to measure it ? | 5M |
Blood
- Blood is a specialized type of connective tissue that circulates throughout the body, serving as a medium for transporting nutrients, gases, and waste products.
- It consists of two major components: plasma (the fluid matrix) and formed elements (cells and cell fragments).
Plasma
- Appearance: A straw-colored, viscous fluid.
- Constitutes: Nearly 55% of blood volume.
- Composition:
- Water (90-92%): Forms the bulk of plasma and serves as a solvent for various substances.
- Proteins (6-8%):
- Fibrinogen: A protein essential for blood clotting.
- Globulins: Involved in the immune response, defense mechanisms.
- Albumins: Help in maintaining osmotic balance (keeping the right amount of water in the blood).
- Minerals: Such as Na+, Ca²+, Mg²+, HCO₃⁻, Cl⁻.
- Nutrients: Glucose, amino acids, lipids, etc., are always in transit in the body.
- Coagulation factors: Present in an inactive form; essential for clotting when activated.
- Serum: Plasma without the clotting factors is called serum.
Formed Elements of Blood
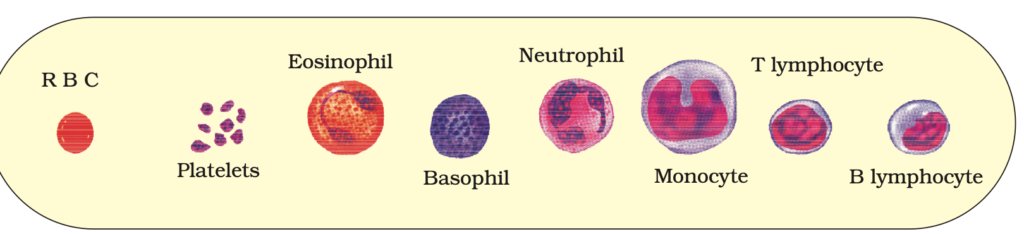
The formed elements of blood refer to the cellular components: erythrocytes (red blood cells, RBCs), leucocytes (white blood cells, WBCs), and platelets. Together, they make up nearly 45% of the blood.
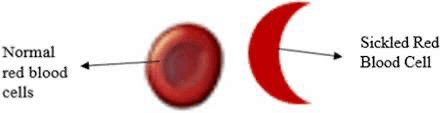
1. Erythrocytes (Red Blood Cells – RBCs)
- Abundance: RBCs are the most numerous cells in the blood, with a healthy adult having 5 to 5.5 million RBCs/mm³ of blood.
- Formation: They are produced in the red bone marrow of adults.
- Structure:
- Biconcave shape: This shape increases surface area for gas exchange.
- Anucleate: RBCs lack a nucleus in most mammals.
- Color: RBCs are red due to hemoglobin, an iron-containing protein that binds oxygen.
- Hemoglobin Content: A healthy individual has 12-16 grams of hemoglobin per 100 ml of blood.
- Function: Primarily involved in the transportation of respiratory gases (oxygen and carbon dioxide).
- Lifespan: RBCs live for an average of 120 days. After this, they are destroyed in the spleen, often referred to as the “graveyard” of RBCs.
2. Leucocytes (White Blood Cells – WBCs)
- Appearance: WBCs are colorless because they lack hemoglobin.
- Nucleus: They are nucleated (contain a nucleus).
- Abundance: The normal count is around 6,000-8,000 WBCs/mm³ of blood.
- Lifespan: WBCs are generally short-lived compared to RBCs.
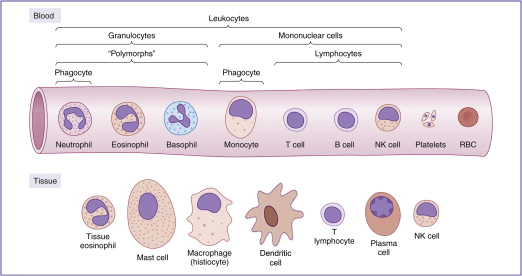
- Categories: WBCs are classified into two main categories:
- Granulocytes (contain granules in the cytoplasm):
- Neutrophils (60-65%): The most abundant WBCs, involved in phagocytosis (engulfing and digesting pathogens).
- Eosinophils: Involved in combating parasitic infections and allergic reactions.
- Basophils (0.5-1%): Least abundant, involved in inflammatory responses and release substances like histamine, serotonin, and heparin.
- Agranulocytes (lack granules in the cytoplasm):
- Lymphocytes (20-25%): Key players in the immune response, with two types:
- B lymphocytes: Produce antibodies.
- T lymphocytes: Involved in directly attacking infected cells.
- Monocytes (6-8%): Large phagocytic cells that engulf pathogens and dead cells.
- Lymphocytes (20-25%): Key players in the immune response, with two types:
- Granulocytes (contain granules in the cytoplasm):
3. Platelets (Thrombocytes)
- Structure: Platelets are cell fragments derived from megakaryocytes in the bone marrow.
- Abundance: Platelet count in the blood ranges from 1,500,000 to 3,500,000 platelets/mm³.
- Function:
- Platelets are essential for blood clotting and wound healing.
- They release various substances involved in the coagulation process, helping to form blood clots to prevent excessive blood loss after injury.
- Disorders: A low platelet count can lead to clotting disorders, causing excessive bleeding.
Hemoglobin
What is Hemoglobin?
- Hemoglobin is a complex protein found in red blood cells (RBCs) that plays a crucial role in oxygen transport and carbon dioxide removal in the body. It is the molecule responsible for giving blood its red color.
Structure of Hemoglobin
- Composition:
- Hemoglobin is a globular protein composed of four subunits:
- Two alpha (α) chains
- Two beta (β) chains (in adult hemoglobin, HbA)
- Each subunit contains a heme group, which has an iron (Fe²⁺) ion at its center.
- Hemoglobin is a globular protein composed of four subunits:
- Heme Group:
- The heme group binds to oxygen (O₂) molecules. One hemoglobin molecule can carry up to four oxygen molecules since it has four heme groups.
- Variants:
- Fetal Hemoglobin (HbF): Found in fetuses; has a higher affinity for oxygen.
- Adult Hemoglobin (HbA): The most common type in adults.
Blood Groups
ABO Blood Grouping System
The ABO blood grouping system is based on the presence or absence of two antigens, A and B, on the surface of the red blood cells (RBCs). The blood plasma of individuals contains natural antibodies, which are proteins produced in response to the antigens that the person does not have.
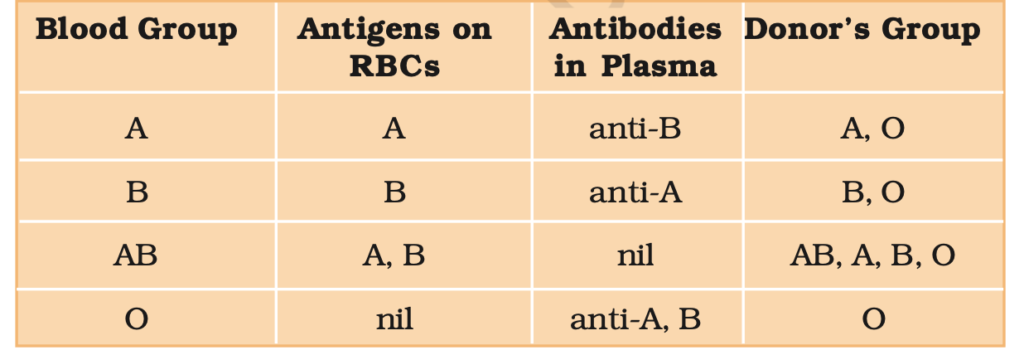
- Group O – Universal Donors:
- Individuals with blood group O can donate blood to anyone with any blood group (A, B, AB, or O).
- This is because O negative blood has no A or B antigens and O positive blood only lacks the Rh antigen, making it compatible with all other blood types.
- Group AB – Universal Recipients:
- People with blood group AB can receive blood from any group (A, B, AB, or O), making them universal recipients.
- This is because individuals with AB blood have both A and B antigens on their red blood cells, so they do not produce antibodies against A, B, or Rh antigens.
ABO Group Compatibility
| Blood Group | Can Receive From | Can Donate To |
| A | A, O | A, AB |
| B | B, O | B, AB |
| AB | A, B, AB, O (universal recipient) | AB |
| O | O | All groups (universal donor) |
Rh Blood Group System
The Rh antigen is another important factor in blood grouping, discovered from studies on Rhesus monkeys (hence the name “Rh”). The Rh factor is present on the surface of red blood cells in the majority (about 80%) of humans.
- Individuals with the Rh antigen on their RBCs are called Rh-positive (Rh+).
- Those who lack the Rh antigen are called Rh-negative (Rh-).
Rh Compatibility and Blood Transfusion:
- Rh+ individuals can receive blood from both Rh+ and Rh- individuals.
- Rh- individuals should receive blood only from Rh- individuals to avoid the formation of anti-Rh antibodies, which could lead to complications in future transfusions.
Rh Factor Compatibility:
| Rh Status | Can Receive From |
| Rh+ | Rh+, Rh- |
| Rh- | Rh- |
Rh Incompatibility in Pregnancy:
Rh incompatibility occurs when an Rh-negative (Rh-) mother is pregnant with an Rh-positive (Rh+) baby. The issue arises due to the following reasons:
- First Pregnancy:
- During the first pregnancy, the placenta usually keeps the maternal and fetal blood separate. Thus, the Rh-negative mother is not exposed to the Rh-positive fetal blood.
- During Delivery:
- During delivery, small amounts of the Rh+ fetal blood may enter the maternal bloodstream, causing the mother’s immune system to produce anti-Rh antibodies. These antibodies specifically target the Rh antigen on red blood cells.
- Subsequent Pregnancies:
- In future pregnancies, if the mother is again carrying an Rh-positive baby, the anti-Rh antibodies from the mother can cross the placenta and attack the Rh-positive fetal red blood cells.
- This leads to destruction of fetal red blood cells (hemolysis), causing severe anemia and jaundice in the baby. In extreme cases, it can lead to death of the fetus or require medical intervention such as a blood transfusion for the newborn.
Erythroblastosis Fetalis/Hemolytic Disease of the Newborn (HDN)
This condition is known as erythroblastosis fetalis, where the fetal red blood cells are destroyed (Hemolysis) due to the Rh incompatibility between the mother and fetus.
Prevention:
- The condition can be prevented by administering anti-Rh antibodies (Rh immunoglobulin) to the Rh-negative mother immediately after the delivery of the first Rh-positive baby.
- This treatment prevents the mother from forming antibodies against Rh, thus protecting future pregnancies.
Trigger:
- If an Rh-negative mother is carrying an Rh-positive fetus (inherited from the father), the mother’s immune system may produce anti-Rh antibodies.
- This usually occurs after exposure to Rh-positive blood, such as during:
- A previous pregnancy with an Rh-positive baby.
- A miscarriage or abortion.
- Blood transfusion with Rh-positive blood.
- Trauma during pregnancy or delivery.
Treatment
- Before Birth
- Intrauterine Transfusion:
- Red blood cells are transfused directly into the fetus to treat severe anemia.
- Early Delivery:
- If the condition is critical, labor may be induced preterm once the fetus is viable.
- Intrauterine Transfusion:
- After Birth:
- Phototherapy:
- Treats jaundice by breaking down excess bilirubin using blue light.
- Exchange Transfusion:
- Replaces the newborn’s blood with donor blood to remove bilirubin and maternal antibodies.
- Intravenous Immunoglobulin (IVIG):
- Reduces antibody-mediated hemolysis.
- Phototherapy:
Blood Transfusion Compatibility
When performing a blood transfusion, it is essential to match the donor’s blood with the recipient’s blood to avoid complications such as agglutination (clumping of RBCs), which can lead to serious health issues.
Blood Transfusion Compatibility Chart
| Blood Type | Can Donate To | Can Receive From |
| O− | All blood types (Universal Donor) | O− |
| O+ | O+, A+, B+, AB+ | O+, O− |
| A− | A+, A−, AB+, AB− | A−, O− |
| A+ | A+, AB+ | A+, A−, O+, O− |
| B− | B+, B−, AB+, AB− | B−, O− |
| B+ | B+, AB+ | B+, B−, O+, O− |
| AB− | AB+, AB− | AB−, A−, B−, O− |
| AB+ | AB+ (Universal Recipient) | All blood types |
Key Points:
- Universal Donor: O− blood can be given to any blood type because it lacks A, B, and Rh antigens, minimizing immune reactions.
- Universal Recipient: AB+ blood can receive from all blood types because it has all antigens (A, B, and Rh), preventing antibody reactions.
Significance of Blood Groups
- Transfusion Medicine: Mismatched transfusions can lead to serious reactions.
- Pregnancy:Rh incompatibility between mother and fetus can lead to hemolytic disease of the newborn (HDN).
- Genetics: Blood groups are inherited and can provide insights into ancestry and population genetics.
- Disease Susceptibility: Some studies link blood groups to certain diseases (e.g., Type O may have lower risk of heart disease, while Type A might have higher susceptibility to stomach cancer).
Functions of blood:
Blood performs a wide range of critical functions in the body, essential for maintaining life. These functions can be broadly categorized into transportation, regulation, and protection:
1. Transportation
Blood serves as the body’s delivery and waste removal system:
- Oxygen Transport: Delivers oxygen from the lungs to tissues and organs via hemoglobin in red blood cells.
- Carbon Dioxide Transport: Carries carbon dioxide, a waste product, from tissues back to the lungs for exhalation.
- Nutrient Transport: Distributes nutrients (e.g., glucose, amino acids, fatty acids) absorbed from the digestive system to cells.
- Waste Removal: Transports metabolic waste products (e.g., urea, creatinine) to the kidneys, liver, and skin for excretion.
- Hormone Distribution: Carries hormones from endocrine glands to target tissues and organs.
- Heat Distribution: Helps in regulating body temperature by distributing heat produced by metabolic processes.
2. Regulation
Blood plays a vital role in maintaining homeostasis:
- pH Balance: Contains buffers, such as bicarbonate ions, to maintain a stable blood pH (around 7.4).
- Fluid Balance: Regulates the movement of water between blood vessels and tissues, maintaining blood pressure and cell hydration.
- Body Temperature: Adjusts heat distribution to maintain a consistent body temperature.
3. Protection
Blood is a key player in the immune system and in protecting the body from injury and infection:
- Clotting Mechanism: Platelets and clotting factors prevent excessive blood loss by forming clots at sites of injury.
- Immune Defense:
- White Blood Cells (Leukocytes): Detect and destroy pathogens like bacteria, viruses, and fungi.
- Antibodies: Produced by B-lymphocytes, these proteins neutralize harmful microorganisms and toxins.
- Complement Proteins: Assist in the destruction of pathogens.
- Removal of Dead Cells and Debris: Monocytes and macrophages help clear cellular debris and dead cells.
Additional Functions
- Gas Exchange: Blood gases (oxygen and carbon dioxide) are continuously exchanged between the lungs and tissues.
- Nutritional Reserve: Plasma proteins can act as a reserve of amino acids in times of need.
- Maintenance of Organ Function: Blood flow ensures that organs receive adequate oxygen and nutrients for optimal function.
Plasma proteins
Plasma proteins are essential components of blood plasma, comprising about 7-9% of its total volume. These proteins play vital roles in maintaining osmotic pressure, transporting substances, immunity, blood clotting, and other physiological functions.
Types of Plasma Proteins
Albumins
- Proportion: ~60% of total plasma proteins.
- Synthesis: Produced in the liver.
- Functions:
- Maintains colloid osmotic pressure, crucial for preventing fluid leakage from blood vessels into tissues.
- Transports substances like
- Hormones (e.g., thyroid hormones, steroid hormones).
- Fatty acids.
- Drugs.
- Acts as a buffer, helping regulate blood pH.
Globulins
- Proportion: ~36% of plasma proteins.
- Types:
- Alpha (α) Globulins:
- Produced by the liver.
- Transport lipids, hormones, and vitamins.
- Include haptoglobin (binds free hemoglobin) and ceruloplasmin (carries copper).
- Beta (β) Globulins:
- Transport iron (e.g., transferrin) and lipids.
- Include complement proteins involved in immunity.
- Gamma (γ) Globulins:
- Produced by plasma cells (B-lymphocytes).
- Represent antibodies (immunoglobulins) essential for immunity.
- Alpha (α) Globulins:
Fibrinogen
- Proportion: ~4% of plasma proteins.
- Synthesis: Produced by the liver.
- Function:
- Plays a critical role in blood clotting.
- Converted into insoluble fibrin during the coagulation cascade, forming the framework of blood clots.
Minor Plasma Proteins
- Prothrombin: A clotting factor converted into thrombin during coagulation.
- Complement Proteins: Part of the immune system; involved in destroying pathogens.
- Enzymes and Hormones: Includes protease inhibitors and regulatory proteins.
Functions of Plasma Proteins
- Osmotic Balance: Albumins help maintain the oncotic pressure, balancing fluid levels between blood vessels and tissues.
- Transport: Bind and carry hormones, lipids, vitamins, and waste products like bilirubin.
- Immune Response: Gamma globulins (antibodies) recognize and neutralize pathogens.
- Blood Clotting: Fibrinogen and other clotting factors prevent excessive bleeding by forming clots.
- Buffering: Stabilize blood pH, maintaining it within the physiological range (7.35–7.45).
- Nutrition: Serve as a reserve supply of amino acids for tissue repair.
Clinical Importance of Plasma Proteins
Abnormal Levels:
- Hypoproteinemia (low plasma protein levels):
- Causes: Malnutrition, liver disease, kidney disease, or chronic blood loss.
- Hyperproteinemia (high plasma protein levels):
- Causes: Chronic inflammation, dehydration, or certain cancers (e.g., multiple myeloma).
Diagnostic Use:
- Measurement of albumin, globulin, and fibrinogen levels helps diagnose conditions like liver disease, kidney disease, and immune disorders.
Immunoglobulins
Immunoglobulins (Ig), also known as antibodies, are specialized glycoproteins produced by B lymphocytes and plasma cells. They play a central role in the immune system by identifying and neutralizing pathogens like bacteria and viruses. Immunoglobulins circulate in the blood and lymph and are also present in secretions such as saliva and mucus.
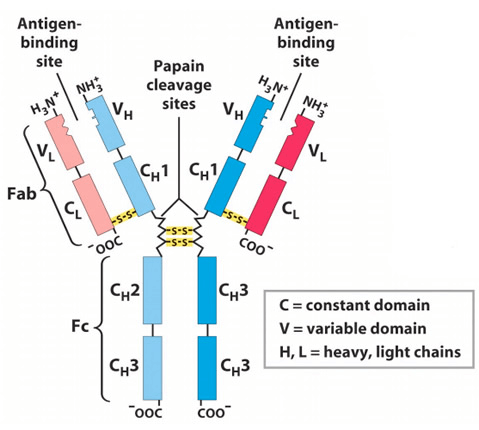
Structure of Immunoglobulins
- Basic Structure: Shaped like a “Y”.
- Composed of: Four polypeptide chains:
- Two heavy (H) chains: Longer and determine the antibody’s class.
- Two light (L) chains: Shorter and identical in all types of immunoglobulins.
- Chains are connected by disulfide bonds.
- Each chain has:
- Variable regions (Fab):
- Located at the tips of the “Y”.
- Contain antigen-binding sites (highly specific to the pathogen).
- Constant regions (Fc):
- The stem of the “Y”.
- Determines the effector functions (e.g., binding to immune cells).
- Variable regions (Fab):
- Composed of: Four polypeptide chains:
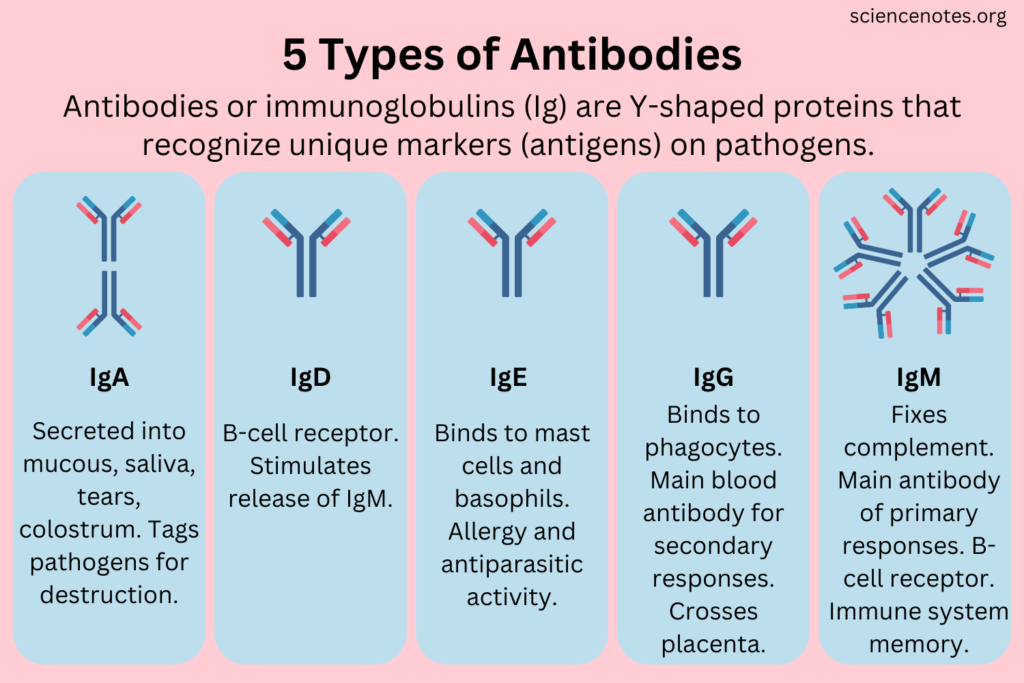
Types of Immunoglobulins
There are five main classes of immunoglobulins, each with specific functions:
1. IgG:
- Proportion: ~75-80% of total antibodies.
- Functions:
- Major antibody in secondary immune response.
- Provides long-term immunity after infection or vaccination.
- Crosses the placenta to protect the fetus.
- Activates complement proteins and enhances phagocytosis.
- Location: Found in blood and extracellular fluid.
2. IgA:
- Proportion: ~10-15% of total antibodies.
- Functions:
- Protects mucosal surfaces (e.g., respiratory and gastrointestinal tracts) by preventing pathogen adherence.
- Found in secretions (saliva, tears, breast milk, mucus).
- Provides passive immunity to newborns through breast milk.
- Location: Primarily in mucosal linings and secretions.
3. IgM:
- Proportion: ~5-10% of total antibodies.
- Functions:
- First antibody produced during an initial immune response.
- Forms large complexes (pentameric structure) to effectively neutralize pathogens.
- Activates the complement system.
- Location: Found in blood and lymph.
4. IgE:
- Proportion: <1% of total antibodies.
- Functions:
- Involved in allergic reactions.
- Binds to allergens and triggers the release of histamine from mast cells and basophils.
- Provides defense against parasitic infections (e.g., helminths).
- Location: Found in tissues and bound to mast cells or basophils.
5. IgD:
- Proportion: <1% of total antibodies.
- Functions:
- Functions as a receptor on the surface of immature B cells.
- Plays a role in the activation and regulation of B cells.
- Location: Found in small amounts in blood and lymph, mostly associated with B cells.
Functions of Immunoglobulins
- Neutralization:
- Bind to toxins, viruses, or bacteria to block their harmful effects.
- Opsonization:
- Coats pathogens to enhance their recognition and engulfment by phagocytes.
- Agglutination:
- Clumps pathogens together for easier elimination.
- Complement Activation:
- Triggers the complement cascade, leading to pathogen destruction.
- Antibody-Dependent Cellular Cytotoxicity (ADCC):
- Binds infected or abnormal cells, signaling their destruction by natural killer (NK) cells.
Clinical Importance of Immunoglobulins
1. Diagnostic Tests:
- Serum antibody levels can help diagnose:
- Infections (e.g., elevated IgM indicates a recent infection).
- Immune deficiencies.
- Autoimmune diseases (e.g., lupus, rheumatoid arthritis).
- Allergic conditions (elevated IgE).
- Tests include ELISA and Western blotting.
2. Immunoglobulin Therapy:
- Intravenous Immunoglobulin (IVIG): Used to treat immune deficiencies, autoimmune disorders, and severe infections.
- Monoclonal Antibodies: Lab-produced antibodies targeting specific diseases (e.g., cancer, rheumatoid arthritis).
Conditions Associated with Immunoglobulins
- Deficiency:
- Hypogammaglobulinemia: Low immunoglobulin levels leading to recurrent infections.
- Agammaglobulinemia: Complete absence of immunoglobulins due to genetic defects.
- Excess:
- Multiple Myeloma: Cancer of plasma cells leading to excessive production of abnormal immunoglobulins.
- Waldenström’s Macroglobulinemia: Overproduction of IgM.
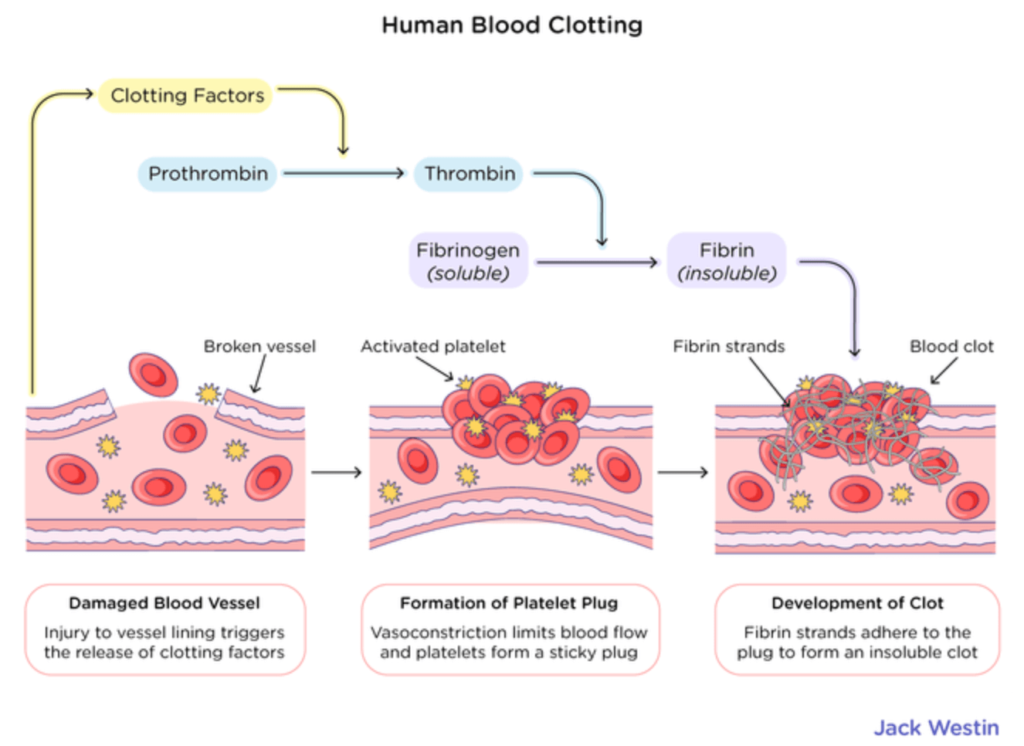
Blood coagulation
Blood coagulation or clotting, is a vital process that prevents excessive blood loss when blood vessels are injured. It involves a series of complex biochemical reactions leading to the formation of a stable blood clot (thrombus).
Phases of Blood Coagulation
1. Vascular Spasm (Vasoconstriction)
- Trigger: Injury to blood vessel
- Effect: Blood vessel constricts to reduce blood flow and minimize blood loss
2. Platelet Plug Formation
- Platelet Activation: Platelets adhere to the exposed collagen at the injury site.
- Platelet Aggregation: Activated platelets release chemicals that attract more platelets, forming a plug.
3. Coagulation Cascade
- Clotting Factors: A series of proteins (I-XIII) are activated in a cascade, leading to the formation of fibrin threads.
- Intrinsic Pathway: Activated by damage to the vessel wall.
- Extrinsic Pathway: Triggered by tissue factor from damaged tissue.
- Factor X Activation: Both pathways lead to Factor X, a key protein in the clotting process.
- Factor X activates prothrombin into thrombin.
- Thrombin converts fibrinogen into fibrin, forming a mesh that stabilizes the clot.
4. Clot Retraction and Repair
- Platelets contract, pulling the clot tighter to seal the wound. Fibrin forms a mesh that holds the clot together and supports tissue healing.
5. Clot Removal (Fibrinolysis)
- Once the wound heals, your body no longer needs the clot. Plasmin, a protein, breaks down the clot in a process called fibrinolysis, cleaning up the area.
Disorders of Coagulation
- Hemophilia:
- Hemophilia A: Deficiency of Factor VIII.
- Hemophilia B: Deficiency of Factor IX.
- Thrombosis:
- Formation of abnormal clots (e.g., in deep veins, leading to deep vein thrombosis or pulmonary embolism).
- Disseminated Intravascular Coagulation (DIC):
- Uncontrolled widespread clotting, exhausting clotting factors and causing severe bleeding.
- Vitamin K Deficiency:
- Impairs synthesis of clotting factors, leading to excessive bleeding.
Blood Group Inheritance
The determination of blood group inheritance follows Mendelian genetics, where parents pass on their blood group alleles (genes) to their children.
- ABO System follows simple Mendelian inheritance with codominance for A and B alleles and recessiveness for O.
- Rh Factor follows a Mendelian inheritance pattern with Rh+ being dominant over Rh-.
- Inheritance patterns can help predict the possible blood group of offspring and identify potential Rh incompatibilities (important during pregnancy).
- Blood group compatibility is crucial for blood transfusions and organ transplants, as mismatches can lead to immune reactions.
ABO Blood Group Inheritance Table
| Parent 1 Blood Type | Parent 2 Blood Type | Possible Offspring Blood Types |
| Type A (IᴬI⁰) | Type A (IᴬI⁰) | A (IᴬI⁰), O (I⁰I⁰) |
| Type A (IᴬI⁰) | Type B (IᴮI⁰) | A (IᴬI⁰), B (IᴮI⁰), AB (IᴬIᴮ), O (I⁰I⁰) |
| Type A (IᴬI⁰) | Type AB (IᴬIᴮ) | A (IᴬI⁰), B (IᴮI⁰), AB (IᴬIᴮ) |
| Type B (IᴮI⁰) | Type B (IᴮI⁰) | B (IᴮI⁰), O (I⁰I⁰), AB (IᴬIᴮ) |
| Type AB (IᴬIᴮ) | Type O (I⁰I⁰) | A (IᴬI⁰), B (IᴮI⁰) |
| Type AB (IᴬIᴮ) | Type AB (IᴬIᴮ) | A (IᴬI⁰), B (IᴮI⁰), AB (IᴬIᴮ), O (I⁰I⁰) |
| Type O (I⁰I⁰) | Type O (I⁰I⁰) | O (I⁰I⁰) |
Rh Factor Inheritance Table
| Parent 1 Rh Factor | Parent 2 Rh Factor | Possible Offspring Rh Status |
| Rh+ (Rh+Rh-) | Rh+ (Rh+Rh-) | Rh+ or Rh- |
| Rh+ (Rh+Rh-) | Rh- (Rh-Rh-) | Rh+ or Rh- |
| Rh+ (Rh+Rh+) | Rh- (Rh-Rh-) | Rh+ |
| Rh- (Rh-Rh-) | Rh- (Rh-Rh-) | Rh- |
FAQ (Previous year questions)
Functions of Blood Platelets (Thrombocytes):
Blood Clotting: Form an initial plug at injury sites to stop bleeding.
Clot Stabilization: Work with fibrin and thrombin to create stable clots.
Wound Healing: Release growth factors to promote tissue repair.
Immune Support: Aid inflammation and activate immune cells against pathogens.
Hemoglobin is the respiratory pigment present in the red blood cells. It has a very high affinity for oxygen. Each hemoglobin molecule can carry four molecules of oxygen.
Haemoglobin is present in red blood cells and transports oxygen from the lungs to the body tissues.
It helps in carrying carbon dioxide from the tissues back to the lungs.
Most of the carbon dioxide is transported in the form of bicarbonates.
Haemoglobin gives red colour to the blood and helps in oxygen transport.
It facilitates the exchange of gases required for cellular respiration.
It also helps in maintaining the pH of blood.
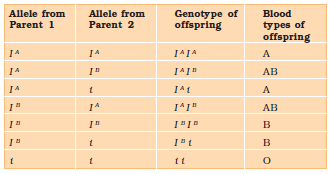
ABO blood groups are controlled by the gene I.
The plasma membrane of red blood cells contains antigens, and the type of antigen is determined by the gene.
The I gene has three alleles:IA, IB and i.
IA: Produces A antigen on red blood cells, giving blood group A.
IB: Produces B antigen, giving blood group B.
i: Produces no antigen, giving blood group O.
Humans are diploid, so they inherit two of the three I gene alleles.
IA and IB are dominant over i, means – When IA and i are present, IA is expressed.
When IB and i are present, IB is expressed.
However, when IA and IB are present together, both express their own types of antigens due to co-dominance. As a result, red blood cells have both A and B types of antigens.
Since there are three different alleles, six possible combinations of these alleles can occur, resulting in six different genotypes for human ABO blood types.
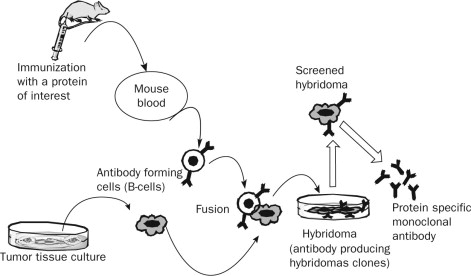
Monoclonal antibodies (mAbs) are antibodies that are made by identical immune cells, all of which are clones of a unique parent cell.
These antibodies are designed to bind specifically to a single epitope of an antigen. This characteristic makes them highly specific and useful in both diagnostic and therapeutic applications.
mAbs are commonly used in the treatment of various diseases, including cancers, autoimmune diseases, and infectious diseases.
Production of Monoclonal Antibodies
The production of monoclonal antibodies involves a technique known as hybridoma technology, which was developed by Georges Köhler and César Milstein in 1975.
This process enables the generation of large quantities of identical antibodies (monoclonal antibodies).
1. Immunization
An animal, often a mouse, is injected with an antigen (substance that triggers the immune response). This prompts the mouse’s immune system to produce antibodies specific to that antigen.
2. Cell Fusion
The B-cells (antibody-producing cells) from the mouse spleen are isolated.
These B-cells are then fused with myeloma cells (cancerous cells that can divide endlessly).
This fusion forms hybridomas—cells that combine the properties of both B-cells (antibody production) and myeloma cells (unlimited division).
3. Selection and Screening
The hybridomas are cultured in a medium that allows only the fused cells (hybridomas) to survive.
These cells are then tested to identify those producing the desired antibody against the target antigen.
4. Cloning
The selected hybridomas are cloned to create a large population of identical cells.
Each clone produces large quantities of the monoclonal antibody of interest.
Purification
The monoclonal antibodies are harvested and purified from the culture medium for use in various applications.
Applications
Limitations
mAbs are used for targeted treatments in cancer, autoimmune diseases, and conditions like rheumatoid arthritis, offering fewer side effects than traditional treatments.
mAbs are vital in detecting infections, pregnancy, and cancer biomarkers.
They help treat or prevent diseases like COVID-19 by neutralizing viral particles.
mAbs are key in producing biotech products, proteins, and vaccines.
Their production is costly, making treatments unaffordable in some regions.
Patients may develop immune responses, especially with non-human derived antibodies.
mAbs are specific to one antigen, limiting their use across diseases.
The use of animal-derived antibodies raises ethical issues related to animal welfare.
Monoclonal antibodies have transformed medicine by offering highly specific, targeted treatments, especially in oncology and immunology.
However, their high production costs, potential for immune reactions, and ethical considerations in their production present challenges that continue to be addressed in ongoing research.
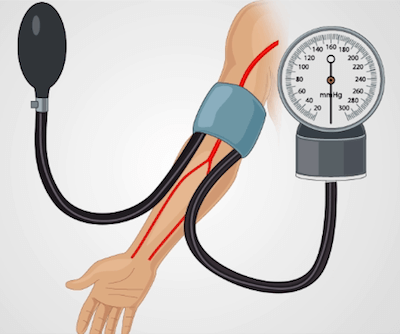
Blood pressure is the force with which blood pushes against the walls of the arteries as the heart pumps it around the body.
It ensures the circulation of blood to deliver oxygen and nutrients to various tissues.
It fluctuates with physical activity, emotions, and health conditions. Proper regulation of blood pressure is essential for overall well-being.
Components:
It is expressed as two values:
Systolic Pressure : Pressure during heartbeats.
Diastolic Pressure: Pressure between heartbeats when the heart relaxes.
Unit of Measurement: millimeters of mercury (mmHg).
Normal Range:
Systolic: 90–120 mmHg
Diastolic: 60–80 mmHg
Normal BP: Around 120/80 mmHg
High Blood Pressure (Hypertension): A reading consistently above 140/90 mmHg.
Low Blood Pressure (Hypotension): A reading consistently below 90/60 mmHg.
Measurement Instrument:
Sphygmomanometer is the standard device used to measure blood pressure.
Types of Sphygmomanometers:
Mercury Sphygmomanometer
Aneroid Sphygmomanometer
Digital Sphygmomanometer
Measurement Site: Measured on the brachial artery of the upper arm.