Human Reproductive System is an essential topic in Biology that explains how humans produce offspring and ensure the continuation of life. It includes specialized organs and processes in both males and females that work together for reproduction.
Human Reproductive System
- Humans are sexually reproducing and viviparous organisms, meaning that they reproduce sexually through the fusion of male and female gametes and give birth to live offspring (instead of laying eggs).
- The reproductive events in humans involve a sequence of processes, which occur after puberty, when individuals reach sexual maturity.
- These processes include gametogenesis (formation of gametes), insemination (transfer of sperm into the female genital tract), fertilization (fusion of male and female gametes), and the subsequent development of the zygote into a fetus through stages like implantation, gestation, and parturition (birth).
The Male Reproductive System
- The male reproductive system is responsible for the production and transport of sperm, and the secretion of male hormones like testosterone.
- It is located in the pelvic region and includes various organs such as testes, accessory ducts, glands, and the external genitalia.
Testes
- The testes (singular: testis) are paired, oval-shaped organs located outside the abdominal cavity within a scrotum. The scrotum serves a crucial function: it maintains the testes at a lower temperature (about 2-2.5°C lower than body temperature), which is essential for the process of spermatogenesis (sperm production).
- Each testis measures approximately 4–5 cm in length and 2–3 cm in width. The outer surface of the testis is covered by a dense connective tissue layer called the tunica albuginea, which provides structural support.
- The interior of each testis is divided into about 250 compartments called testicular lobules. Each lobule contains seminiferous tubules, where sperm are produced.
- The seminiferous tubules are lined with two types of cells:
- Male germ cells (spermatogonia): These cells undergo meiosis to form sperm.
- Sertoli cells: These cells provide nutrients and support to developing sperm cells, ensuring the proper environment for spermatogenesis.
- The interstitial spaces outside the seminiferous tubules contain Leydig cells, which secrete the male sex hormone testosterone. This hormone is essential for the development of male secondary sexual characteristics like facial hair and deep voice, and it plays a key role in regulating sperm production.
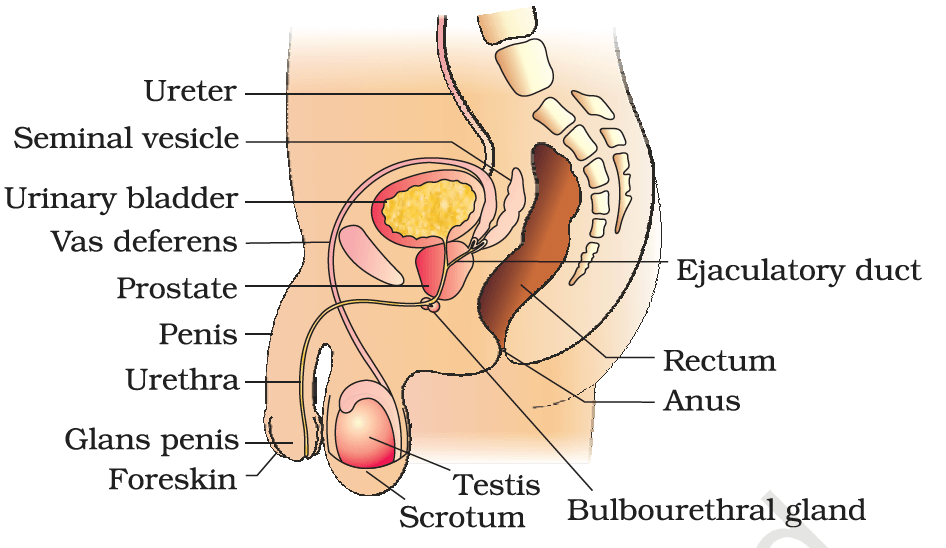
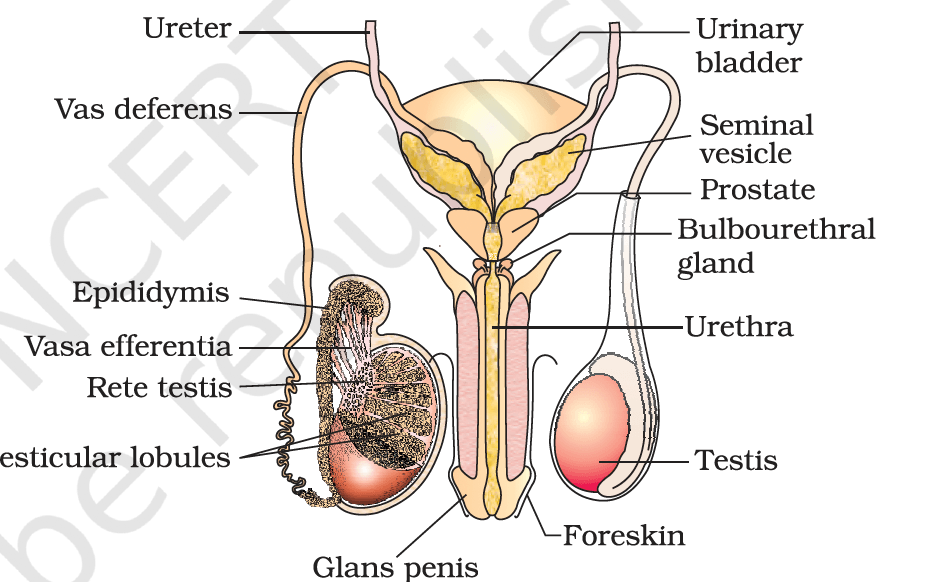
Accessory Ducts
The male reproductive system includes a series of ducts that transport sperm from the testes to the outside of the body:
- Rete testis: This network of tubules collects sperm from the seminiferous tubules.
- Vasa efferentia: These are small tubes that transport sperm from the rete testis to the epididymis.
- Epididymis: The epididymis is a coiled tube located on the posterior side of each testis. It serves as a storage area where sperm mature and gain the ability to swim, a process called sperm maturation.
- Vas deferens: The vas deferens is a long muscular tube that ascends from the epididymis and carries sperm through the pelvic cavity. It loops over the urinary bladder and connects to the urethra via the ejaculatory duct.
Penis and Urethra
- The penis is the male external genital organ. It is made of erectile tissue that allows the penis to become erect during sexual arousal, facilitating the transfer of sperm into the female reproductive tract during insemination.
- The urethra is a tube that runs through the penis and carries both urine and semen to the outside. The opening of the urethra at the tip of the penis is called the urethral meatus.
Male Accessory Glands
These glands produce the seminal plasma that nourishes and helps in the transport of sperm:
- Seminal Vesicles: These paired glands secrete a fluid rich in fructose, calcium, and enzymes. This fluid constitutes the majority of the semen and provides energy for sperm motility.
- Prostate Gland: The prostate secretes a slightly alkaline fluid that helps neutralize the acidic environment of the vagina, ensuring sperm survival. This gland also contributes to the fluid that makes up semen.
- Bulbourethral Glands: These paired glands secrete a clear, lubricating fluid that helps to neutralize any residual acidity in the urethra and facilitates smoother passage of sperm during ejaculation.
The Female Reproductive System
- The female reproductive system is designed to support the processes of ovulation, fertilization, pregnancy, birth, and child care.
- It is made up of several organs that work together to facilitate reproduction. These include the ovaries, oviducts (fallopian tubes), uterus, cervix, vagina, and external genitalia.
- The system also includes mammary glands, which are responsible for lactation and feeding the offspring after birth.
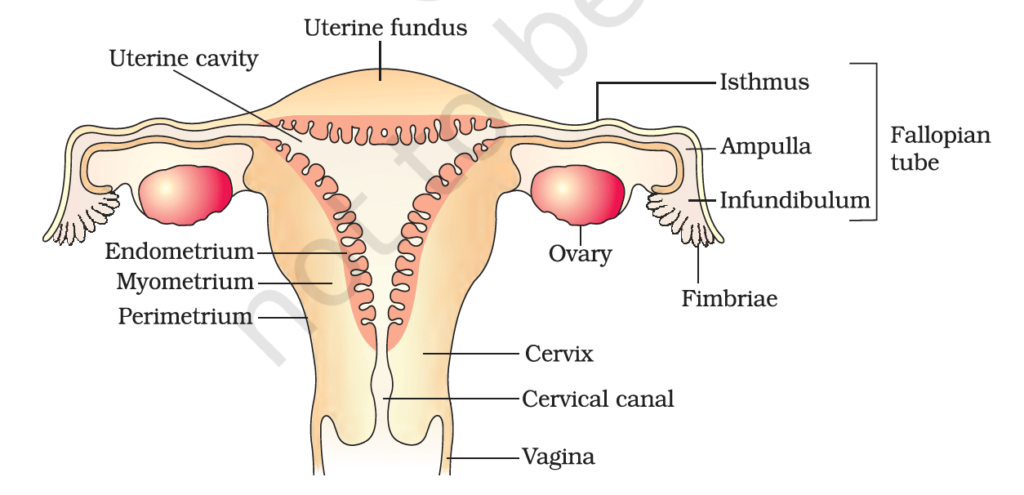
Ovaries: The Primary Female Sex Organs
- Location: The ovaries are paired organs located on either side of the uterus in the lower abdomen, held in place by ligaments.
- Structure: Each ovary is about 2-4 cm in length and has an outer covering called the germinal epithelium, beneath which lies the ovarian stroma. The stroma is divided into two regions:
- Cortex: This is the outer layer of the ovary where ova (eggs) are produced and stored in follicles.
- Medulla: The inner part of the ovary contains blood vessels, nerves, and connective tissue.
- Function: The primary function of the ovaries is to produce ova (female gametes) and to secrete the female hormones estrogen and progesterone, which regulate the menstrual cycle and other reproductive functions.
- Oogenesis (formation of ova) begins before birth and is completed during the female’s reproductive years. At birth, a female has all the eggs she will ever have. These eggs mature in cycles, and only one egg (sometimes more, in the case of twins or multiples) is released during ovulation each month.
Oviducts (Fallopian Tubes): Passage for Eggs
- Structure and Function: Each oviduct (fallopian tube) is a muscular tube, about 10-12 cm in length, that connects the ovaries to the uterus.
- Infundibulum: The funnel-shaped end of the fallopian tube, closest to the ovary, is called the infundibulum. The infundibulum has fimbriae (finger-like projections) that help to catch the ovum (egg) once it is released during ovulation.
- Ampulla: The wider part of the oviduct, where fertilization usually occurs. Sperm meet the egg here to form a zygote.
- Isthmus: The narrow portion of the fallopian tube that connects the ampulla to the uterus.
- The fallopian tubes are the site of fertilization, where sperm and egg meet. The fertilized egg then travels down the tube to implant in the uterus.
Uterus (Womb): Site of Fetal Development
- Location and Structure: The uterus is a pear-shaped, hollow organ located in the pelvic cavity, behind the bladder and in front of the rectum.
- Perimetrium: The thin outer layer, which provides protection.
- Myometrium: The thick, muscular middle layer, responsible for uterine contractions during menstruation and childbirth.
- Endometrium: The inner lining of the uterus, which thickens in preparation for implantation of the fertilized egg. If implantation does not occur, the endometrial lining is shed during menstruation.
- Function: The uterus plays a crucial role in pregnancy, providing a safe environment for the fertilized egg to develop into a fetus. The uterus also contracts during labor to help expel the baby.
Cervix and Vagina: Birth Canal
- Cervix: The cervix is the narrow, lower portion of the uterus that connects to the vagina. It plays a significant role in the menstrual cycle, providing an opening through which menstrual blood flows out of the body. During pregnancy, the cervix remains closed to hold the fetus in place. During labor, it dilates (widens) to allow the baby to pass through the birth canal.
- Vagina: The vagina is a muscular tube that serves as both the birth canal and the passage for menstrual blood and other fluids. The vagina is lined with a mucous membrane that protects it from infection and friction. During sexual intercourse, the vagina accommodates the penis and is the site for sperm deposition.
External Genitalia (Vulva)
The external genitalia of females, collectively called the vulva, includes:
- Mons Pubis: A mound of fatty tissue covered by skin and pubic hair, located above the vaginal opening.
- Labia Majora: These are the outer, fleshy folds of tissue that protect the vaginal opening and urethra.
- Labia Minora: These are the inner folds of tissue, located beneath the labia majora. The labia minora are highly sensitive and provide protection for the vaginal and urethral openings.
- Clitoris: A small, sensitive organ located at the upper junction of the labia minora. It is highly innervated and is an important site for sexual pleasure.
- Hymen: A thin membrane that partially covers the vaginal opening in some females. The hymen may be torn due to sexual intercourse, physical activity, or tampon use, but it is not a reliable indicator of virginity.
Mammary Glands: Milk Production
- Structure: The mammary glands are paired structures, also known as breasts, that produce milk for the nourishment of the newborn. Each breast is made up of glandular tissue and adipose (fat) tissue. The glandular tissue is divided into 15-20 mammary lobes, which contain alveoli, the milk-producing cells.
- Alveoli: These clusters of cells secrete milk, which is stored in the cavities of the alveoli.
- The milk is transported through mammary tubules into mammary ducts, which converge to form a mammary ampulla. The milk then flows into the lactiferous ducts, which lead to the nipple for breastfeeding.
- Function: After childbirth, the mammary glands are activated to produce milk, a process known as lactation. The milk nourishes the infant during the early stages of life, providing essential nutrients and antibodies.
Gametogenesis
Formation of Male and Female Gametes
- Gametogenesis is the biological process by which gametes (sperm in males and ovum in females) are formed in the primary sex organs: the testes in males and the ovaries in females.
- This process ensures the formation of haploid gametes, essential for maintaining the chromosomal number in sexually reproducing organisms.
- Gametogenesis involves spermatogenesis in males and oogenesis in females.
Spermatogenesis: Formation of Male Gametes
- Spermatogenesis is the process of sperm formation that occurs within the seminiferous tubules of the testes, beginning at puberty and continuing throughout life. It can be divided into several stages:
1. Proliferation and Mitosis
- Inside the seminiferous tubules, spermatogonia (immature male germ cells) are located near the basement membrane.
- Spermatogonia are diploid (46 chromosomes) and undergo repeated mitotic divisions to multiply and form a pool of cells.
- Some spermatogonia differentiate into primary spermatocytes, which are destined to undergo meiosis.
2. Meiosis
- First Meiotic Division:
- Each primary spermatocyte (diploid, 46 chromosomes) undergoes the first meiotic division to form two secondary spermatocytes (haploid, 23 chromosomes each).
- Second Meiotic Division:
- Each secondary spermatocyte undergoes the second meiotic division to produce four spermatids, which are haploid and genetically unique.
3. Spermiogenesis
- The spermatids undergo morphological and structural changes to transform into spermatozoa (sperms).
- During this process:
- The nucleus condenses, becoming compact and streamlined.
- The acrosome, a cap-like structure filled with enzymes, develops at the anterior end to help the sperm penetrate the ovum.
- A flagellum forms at the posterior end for motility.
- Mitochondria concentrate in the middle piece to provide energy for movement.
4. Spermiation
- Mature spermatozoa are released from the supporting Sertoli cells into the lumen of the seminiferous tubules.
Hormonal Regulation
- The initiation and regulation of spermatogenesis depend on hormonal signals: GnRH (Gonadotropin-releasing hormone) from the hypothalamus stimulates the anterior pituitary to release:
- LH (Luteinizing Hormone): Stimulates Leydig cells in the interstitial spaces to produce androgens(testosterone), which promote spermatogenesis.
- FSH (Follicle-Stimulating Hormone): Acts on Sertoli cells, stimulating them to secrete factors that support spermatid maturation.
Structure of a Sperm:
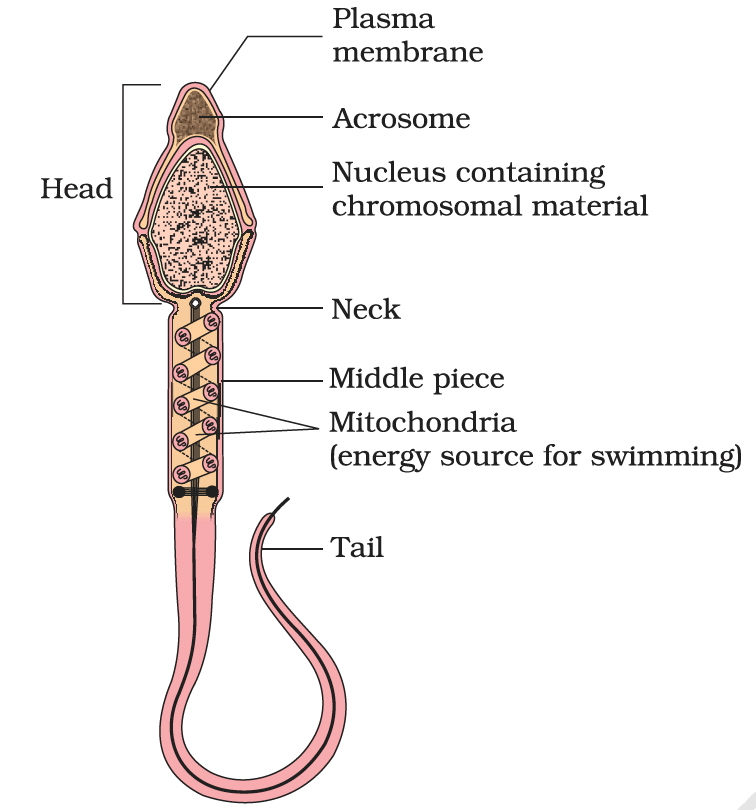
- Head: Contains the haploid nucleus (23 chromosomes) and is capped by the acrosome, which contains enzymes to facilitate penetration of the ovum.
- Middle Piece: Packed with mitochondria, providing the energy needed for motility.
- Tail: A long flagellum that propels the sperm forward.
Seminal Plasma and Semen
- Sperms are transported through the accessory ducts (epididymis, vas deferens, ejaculatory duct) and mixed with secretions from the accessory glands (seminal vesicles, prostate gland, bulbourethral glands) to form semen.
- Seminal plasma provides nutrients, lubrication, and an optimal environment for sperm survival and motility.
Oogenesis:
Formation of Female Gametes
- Oogenesis is the process by which the female gamete (ovum) is produced in the ovaries. Unlike spermatogenesis, which is continuous throughout life, oogenesis begins during fetal development, pauses, and resumes at puberty.
1. Fetal Stage: Formation of Primary Oocytes
- During fetal development, oogonia (female germ cells) divide mitotically to form millions of cells.
- These cells enter prophase-I of meiosis I and pause, becoming primary oocytes.
- Each primary oocyte is surrounded by granulosa cells, forming a primary follicle.
2. Postnatal and Puberty Stage
- A large number of primary oocytes degenerate during childhood, leaving about 60,000–80,000 primary follicles in each ovary by puberty.
- At puberty, under hormonal influence, some primary follicles grow into secondary follicles, characterized by additional layers of granulosa cells and a theca layer.
3. Formation of Secondary Oocyte
- Tertiary Follicle Formation:
- The secondary follicle develops into a tertiary follicle, distinguished by a fluid-filled cavity called the antrum.
- The primary oocyte within the tertiary follicle completes meiosis I, producing:
- A large, nutrient-rich secondary oocyte (haploid).
- A small first polar body that may degenerate or divide.
- The tertiary follicle matures into a Graafian follicle, which ruptures to release the secondary oocyte during ovulation.
4. Ovulation and Meiosis II
- The secondary oocyte remains arrested in metaphase-II of meiosis II.
- If fertilization occurs, meiosis II completes, producing:
- A mature ovum (haploid).
- A second polar body.
- If fertilization does not occur, the secondary oocyte degenerates.
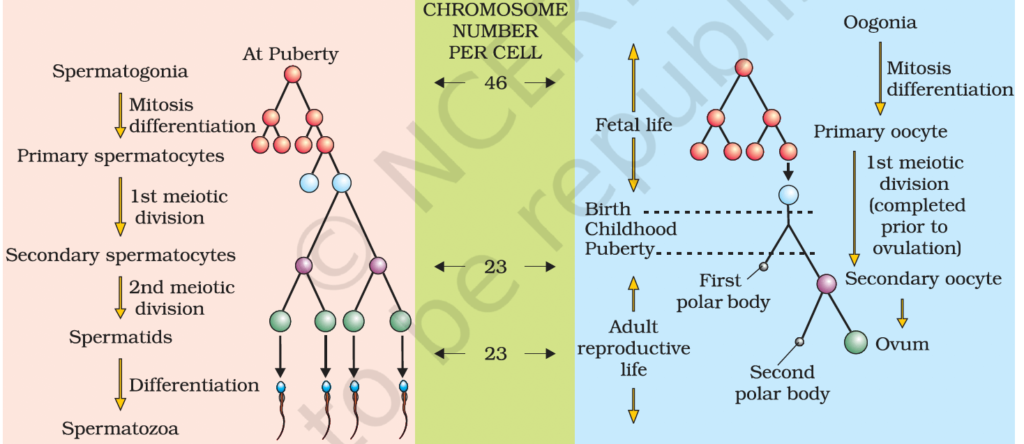
Comparison of Spermatogenesis and Oogenesis
| Aspect | Spermatogenesis | Oogenesis |
| Starting Point | Begins at puberty | Begins during fetal development |
| Duration | Continuous throughout life | Cyclical; limited number of oocytes |
| Output per Cycle | Four functional sperms from one spermatogonium | One ovum and polar bodies from one oogonium |
| Cytoplasm Distribution | Equal distribution among spermatids | Unequal; cytoplasm retained in secondary oocyte |
| Completion of Meiosis | Occurs before release (spermiation) | Meiosis II completes only after fertilization |
| Hormonal Regulation | LH and FSH stimulate Leydig and Sertoli cells | LH and FSH regulate follicular development and ovulation |
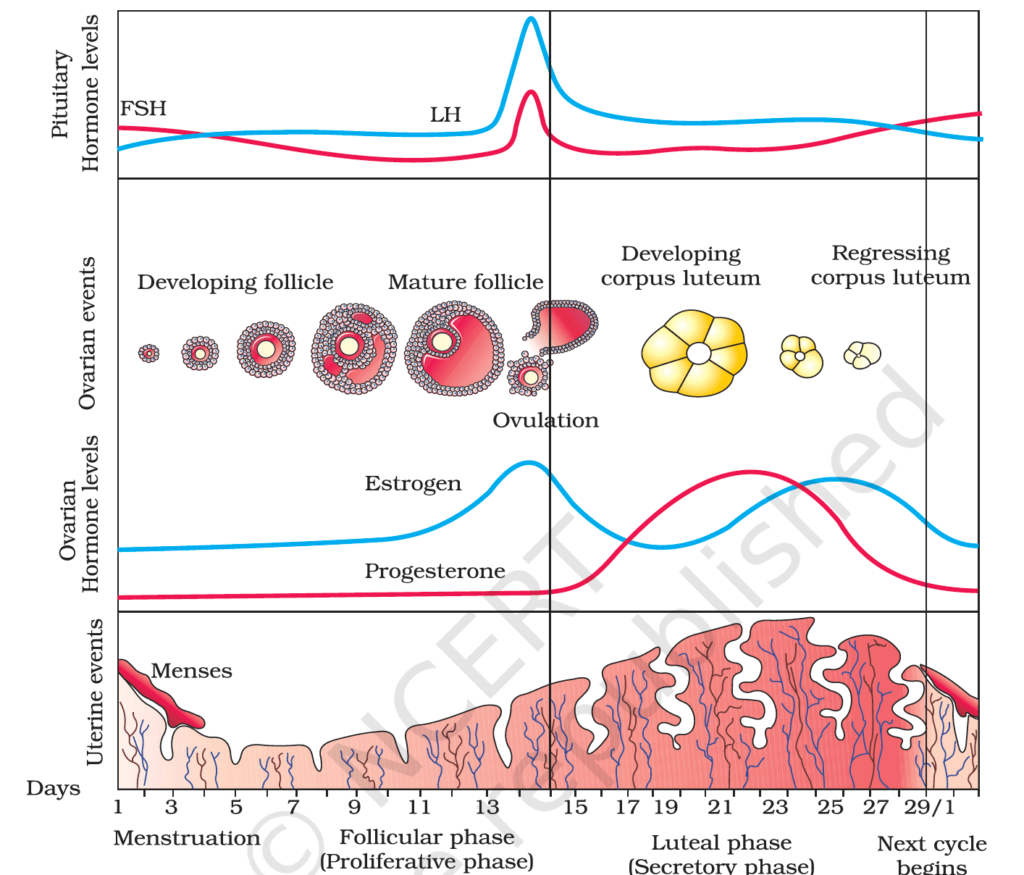
Menstrual Cycle:
A Cyclic Phenomenon of Female Reproductive Physiology
- The menstrual cycle is the reproductive cycle in female primates, including humans, monkeys, and apes. It prepares the female body for potential pregnancy through the regular and periodic maturation and release of an ovum, accompanied by changes in the uterus to support implantation.
- The cycle, which averages 28–29 days, starts with menarche (the first menstruation) at puberty and ends with menopause around the age of 45–55.
Phases of the Menstrual Cycle
The menstrual cycle can be divided into four distinct phases, each marked by physiological, hormonal, and structural changes in the ovaries and uterus:
1. Menstrual Phase (Day 1–5)
- Shedding of the functional layer of the endometrium (the uterine lining) occurs, resulting in bleeding.
- The menstrual blood contains disintegrated endometrial tissue, blood vessels, and unfertilized ovum.
- Hormonal Changes:
- Levels of progesterone and estrogen are at their lowest, causing the endometrium to slough off.
- This triggers the release of GnRH from the hypothalamus, initiating the next cycle.
2. Follicular (Proliferative) Phase (Day 6–13)
- Growth of new follicles in the ovaries begins under the influence of Follicle-Stimulating Hormone (FSH).
- The follicles produce estrogen, which stimulates the regeneration and thickening of the endometrial lining.
- The dominant follicle matures into a Graafian follicle.
- Features:
- The endometrium starts proliferating.
- Estrogen levels rise steadily.
- The body prepares for potential ovulation.
3. Ovulatory Phase (Day 14)
- A surge in Luteinizing Hormone (LH) occurs due to positive feedback from high estrogen levels, triggering ovulation.
- The mature Graafian follicle ruptures, releasing a secondary oocyte into the fallopian tube.
- Features:
- This phase is the most fertile period of the cycle.
- Ovulation is often accompanied by a slight increase in basal body temperature.
4. Luteal (Secretory) Phase (Day 15–28)
- The ruptured Graafian follicle transforms into the corpus luteum, which secretes progesterone.
- Progesterone prepares the endometrium for implantation by making it highly vascularized and glandular.
- If fertilization occurs:
- The corpus luteum persists and continues producing hormones to maintain the pregnancy.
- If fertilization does not occur:
- The corpus luteum degenerates into a corpus albicans.
- Hormone levels drop, leading to the breakdown of the endometrium and the start of a new cycle.
- Features:
- Progesterone dominates this phase.
- The uterus is in its most receptive state for implantation.
Hormonal Regulation of the Menstrual Cycle
The menstrual cycle is tightly controlled by hormonal feedback loops between the hypothalamus, pituitary gland, and ovaries.
- Gonadotropin-Releasing Hormone (GnRH):
- Released by the hypothalamus.
- Stimulates the anterior pituitary to secrete FSH and LH.
- Follicle-Stimulating Hormone (FSH):
- Stimulates the growth of ovarian follicles.
- Promotes estrogen secretion by follicles.
- Luteinizing Hormone (LH):
- Triggers ovulation.
- Stimulates the formation and maintenance of the corpus luteum.
- Estrogen:
- Secreted by growing follicles.
- Promotes endometrial proliferation and positive feedback for the LH surge.
- Progesterone:
- Secreted by the corpus luteum.
- Maintains the endometrium and inhibits FSH and LH to prevent further ovulation during the luteal phase.
Fertilization and Implantation:
Fertilization and implantation are critical events in the establishment of pregnancy. These processes ensure the fusion of gametes and the successful embedding of the developing embryo into the uterine lining.
1. Fertilization
- Fertilization is the fusion of a sperm with an ovum, leading to the formation of a diploid zygote. It occurs in the ampullary region of the fallopian tube, a specific area where the sperm and ovum meet.
Steps in Fertilization:
- Insemination:
- During coitus, semen is released into the vagina through the penis. This process is called insemination.
- Semen contains millions of motile sperms, which swim through the cervix into the uterus and eventually reach the ampullary region of the fallopian tube.
- Ovulation:
- Simultaneously, the ovary releases a secondary oocyte into the fallopian tube. For fertilization to occur, both sperm and ovum must be present in the ampullary region at the same time.
- Sperm Penetration:
- The sperm encounters the ovum’s zona pellucida, a glycoprotein-rich protective layer.
- Enzymes released from the acrosome of the sperm digest the zona pellucida, enabling one sperm to penetrate the ovum’s plasma membrane.
- Cortical Reaction:
- Contact with the zona pellucida triggers a cortical reaction in the ovum, preventing polyspermy (entry of additional sperms).
- Completion of Meiosis:
- The sperm’s entry induces the secondary oocyte to complete its second meiotic division, forming a haploid ovum and a second polar body.
- Zygote Formation:
- The haploid nuclei of the sperm and ovum fuse to form a diploid zygote (46 chromosomes). This marks the beginning of a new individual.
- The zygote’s sex is determined at this stage:
- XX → Female
- XY → Male
- The sex of the baby depends on whether the fertilizing sperm carries an X or Y chromosome. Thus, the father determines the baby’s sex.
2. Cleavage and Early Embryonic Development
- As the zygote travels through the fallopian tube towards the uterus, it undergoes a series of mitotic divisions known as cleavage.
Stages of Cleavage:
- Blastomere Formation:
- The zygote divides into 2, then 4, 8, and 16 cells, forming smaller cells called blastomeres.
- Morula:
- The 8–16 cell stage is termed the morula, a solid ball of cells.
- Blastocyst Formation:
- The morula continues dividing and differentiates into a blastocyst.
- The blastocyst consists of:
- Trophoblast: The outer layer of cells, which will form the placenta.
- Inner Cell Mass: A group of cells inside the blastocyst that will develop into the embryo
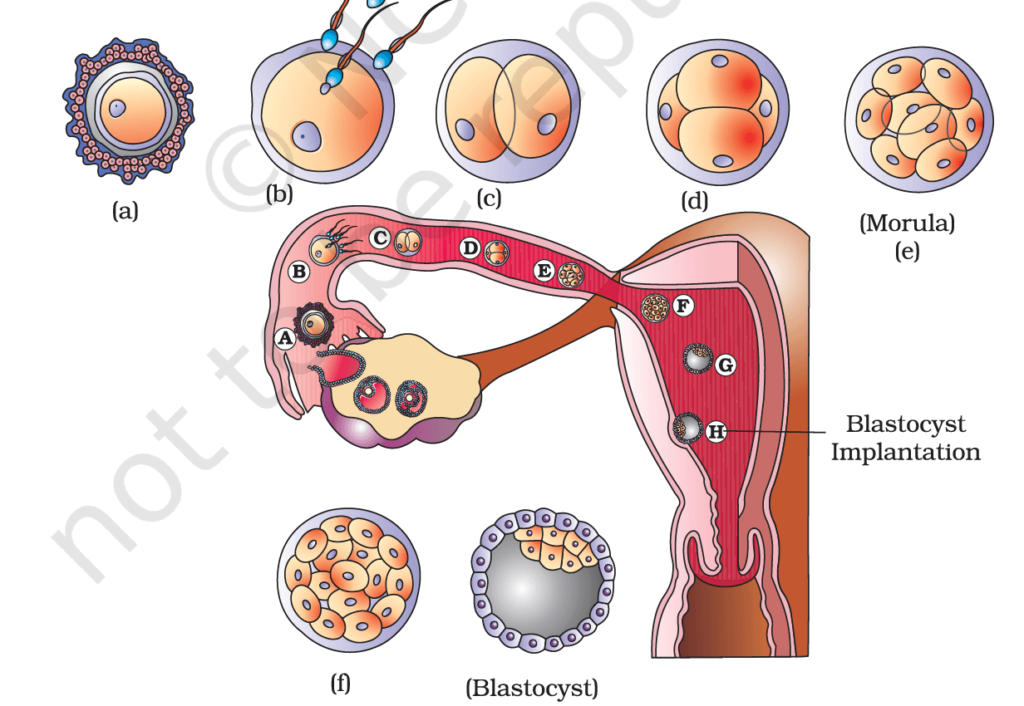
3. Implantation
- Implantation is the process by which the blastocyst embeds itself into the endometrium of the uterus. It establishes a physical and nutritional connection between the mother and the developing embryo.
Steps in Implantation:
- Attachment:
- The trophoblast layer of the blastocyst attaches to the endometrium.
- Invasion:
- The trophoblast cells invade the endometrial tissue, ensuring a secure anchorage.
- Embedding:
- The uterine cells proliferate and grow over the blastocyst, completely embedding it within the endometrial lining.
- Initiation of Pregnancy:
- Implantation marks the beginning of pregnancy. The developing embryo begins to derive nutrients from the maternal blood supply.
