Respiratory System: In Biology, the respiratory system is an essential organ system that helps living beings breathe. It allows the exchange of gases by taking in oxygen and releasing carbon dioxide, which is vital for survival.
Respiratory system
The respiratory system is responsible for the exchange of gases between the body and the environment. This system allows the body to take in oxygen, which is essential for cellular functions, and remove carbon dioxide, which is a waste product of cellular metabolism.
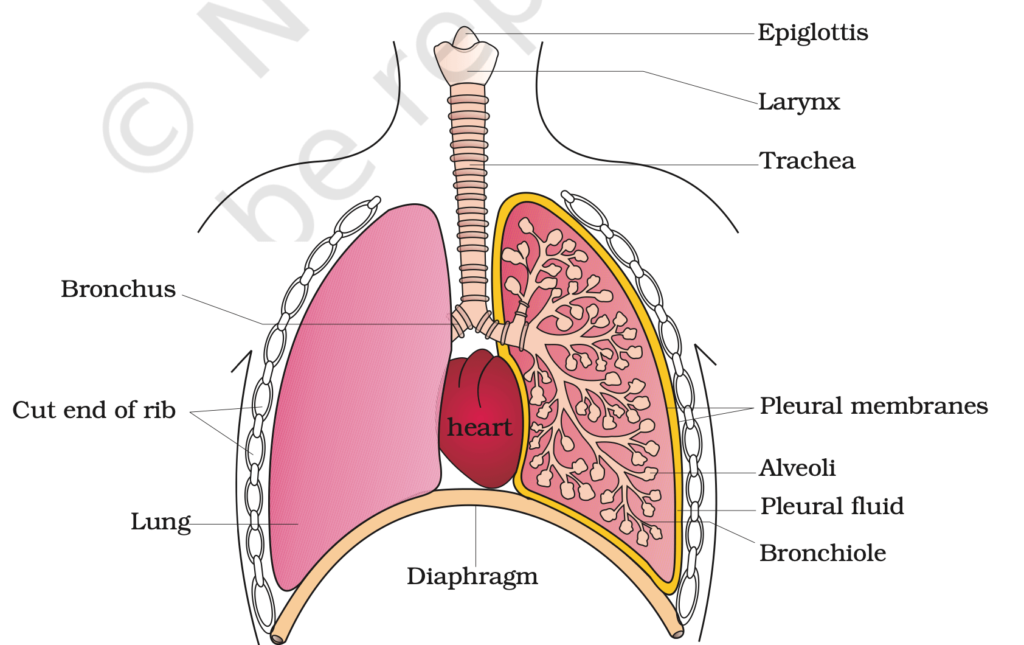
Components of the Respiratory System
It can be divided into two parts: the upper respiratory tract and the lower respiratory tract,
Upper Respiratory Tract
- Nostrils (External Nares): The external openings through which air enters the respiratory system.
- Nasal Cavity: The cavity behind the nostrils that filters, warms, and moistens the incoming air. It is lined with mucus and cilia to trap dust, pathogens, and other particles.
- Pharynx (Throat): A muscular tube that serves as a passage for both air and food. The pharynx is divided into three parts:
Lower Respiratory Tract
- Larynx (Voice Box):
- Contains the vocal cords and plays a role in sound production.
- Acts as a passage for air to the trachea.
- Epiglottis:
- A flap of tissue that prevents food from entering the larynx during swallowing.
- Trachea (Windpipe):
- A tube that connects the larynx to the bronchi.
- Reinforced with C-shaped cartilage rings to keep it open.
- Bronchi:
- Two primary bronchi (left and right) branch from the trachea and lead to each lung.
- Divide further into secondary and tertiary bronchi.
- Bronchioles:
- Smaller branches of the bronchi without cartilage, containing smooth muscles.
- Regulate airflow into the lungs.
Alveoli
- Tiny, sac-like structures at the ends of bronchioles where gas exchange occurs.
- Surrounded by capillaries to facilitate oxygen diffusion into the blood and carbon dioxide diffusion out of the blood.
Lungs
- The lungs are the main organs of respiration, located within the thoracic cavity (chest).
- The lungs are spongy and are responsible for exchanging oxygen and carbon dioxide.
- Each lung is divided into lobes (three lobes on the right, two on the left) and is surrounded by the pleura (A double-layered membrane).
Process of Respiration in Humans:
Respiration in humans involves two main phases: External Respiration (Breathing and gas exchange) and Cellular Respiration (energy production in cells).
External Respiration:
- Inhalation (Inspiration): Oxygen is taken into the lungs through the nose/mouth, trachea, bronchi, and bronchioles, reaching the alveoli.
- Gas Exchange: In the alveoli, oxygen diffuses into the blood, and carbon dioxide diffuses out into the lungs.
- Exhalation (Expiration): Carbon dioxide is expelled from the lungs.
Cellular Respiration:
Occurs inside cells to produce energy (ATP) and has the following steps:
- Glycolysis (in the cytoplasm): Glucose is broken into pyruvate, yielding 2 ATP.
- Krebs Cycle (in mitochondria): Pyruvate is broken down, releasing carbon dioxide, NADH, FADH₂, and 2 ATP.
- Electron Transport Chain (ETC) (in mitochondria): Electrons from NADH and FADH₂ produce water and ~34 ATP through oxidative phosphorylation.
Overall Equation:
C₆H₁₂O₆ (Glucose) + 6O₂ → 6CO₂ + 6H₂O + Energy (38 ATP)
IN DETAIL →
Mechanisms of Breathing:
Breathing, or pulmonary ventilation, involves two processes: inspiration (inhalation) and expiration (exhalation).These processes rely on the creation of a pressure gradient between the atmosphere and the lungs.
Inspiration (Inhalation):
- Inspiration is the process of taking in atmospheric air. The primary muscles involved in inspiration are the diaphragm and the external intercostal muscles.
- Diaphragm: The diaphragm is a dome-shaped muscle that separates the chest (thoracic) cavity from the abdominal cavity.
- External Intercostal Muscles: These muscles are located between the ribs.
- Diaphragm contracts ↓, external intercostals contract
- Thoracic & lung volumes ↑
- Intrapulmonary pressure ↓ → air rushes in
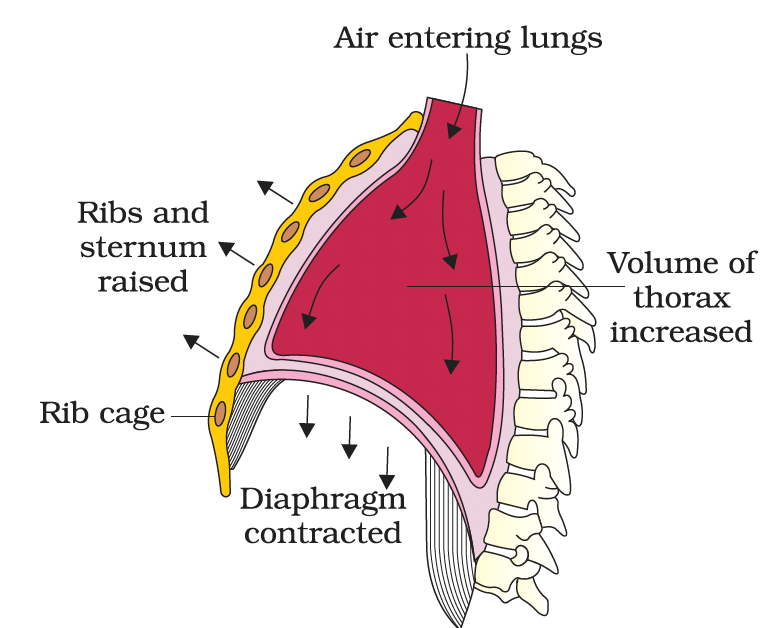
Mechanism of breathing : inspiration
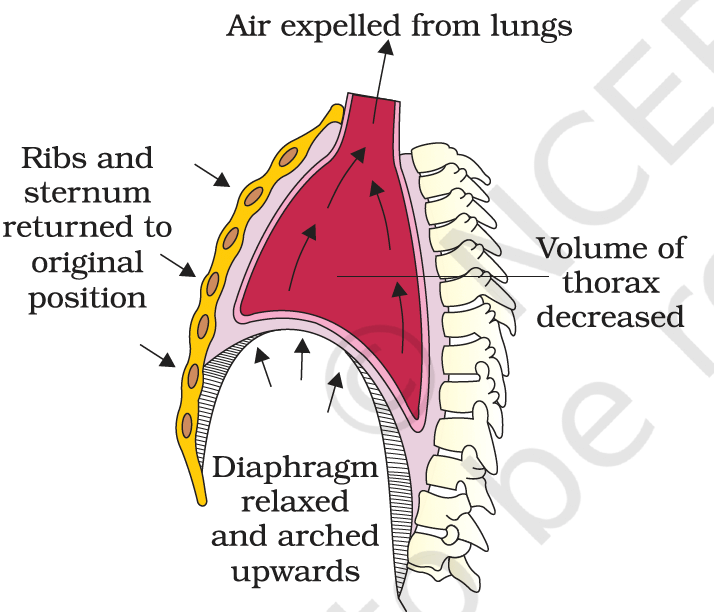
Expiration (Exhalation):
- Diaphragm & intercostals relax → diaphragm moves upward, ribs drop → ↓ thoracic volume
- ↓ lung volume → ↑ intra-pulmonary pressure (higher than atmospheric pressure) → Air is forced out
- Passive vs. Active Expiration:
- Normal expiration is passive, relying on the elastic recoil of lung tissues.
- During vigorous activity, expiration becomes active, involving contraction of internal intercostal and abdominal muscles.
Respiratory Volumes and Capacities
Respiratory Volumes and Capacities
Respiratory Volumes:
- Tidal Volume (TV): The amount of air inhaled or exhaled during normal breathing (~500 mL).
- Total air volume per minute (Minute ventilation) in a healthy individual: ~6000-8000 mL.
- Inspiratory Reserve Volume (IRV): The additional air that can be inhaled forcefully after normal inspiration (~2500–3000 mL).
- Expiratory Reserve Volume (ERV): The additional air that can be exhaled forcefully after normal expiration (~1000 mL).
- Residual Volume (RV): The air remaining in the lungs after maximal exhalation (~1100–1200 mL).
Respiratory Capacities:
- Inspiratory Capacity (IC):
- Total air inspired after normal expiration.
- IC = TV + IRV
- Expiratory Capacity (EC):
- Total air expired after normal inspiration.
- EC = TV + ERV
- Functional Residual Capacity (FRC):
- Air remaining in lungs after normal expiration.
- FRC = ERV + RV
- Vital Capacity (VC):
- Maximum air inhaled after forced expiration OR maximum air exhaled after forced inspiration.
- VC = ERV + TV + IRV
- Total Lung Capacity (TLC):
- Total air lungs can hold after forced inspiration.
- TLC = RV + ERV + TV + IRV
- Alternatively: TLC = VC + RV
Gas Exchange
Exchange of Gases (Respiratory Gas Exchange)
- The exchange of gases (O₂ and CO₂) occurs across the alveolar-capillary membrane through the process of diffusion. The direction of gas diffusion depends on the partial pressure gradients of the gases in different locations. Gas exchange also takes place between the blood and tissues.
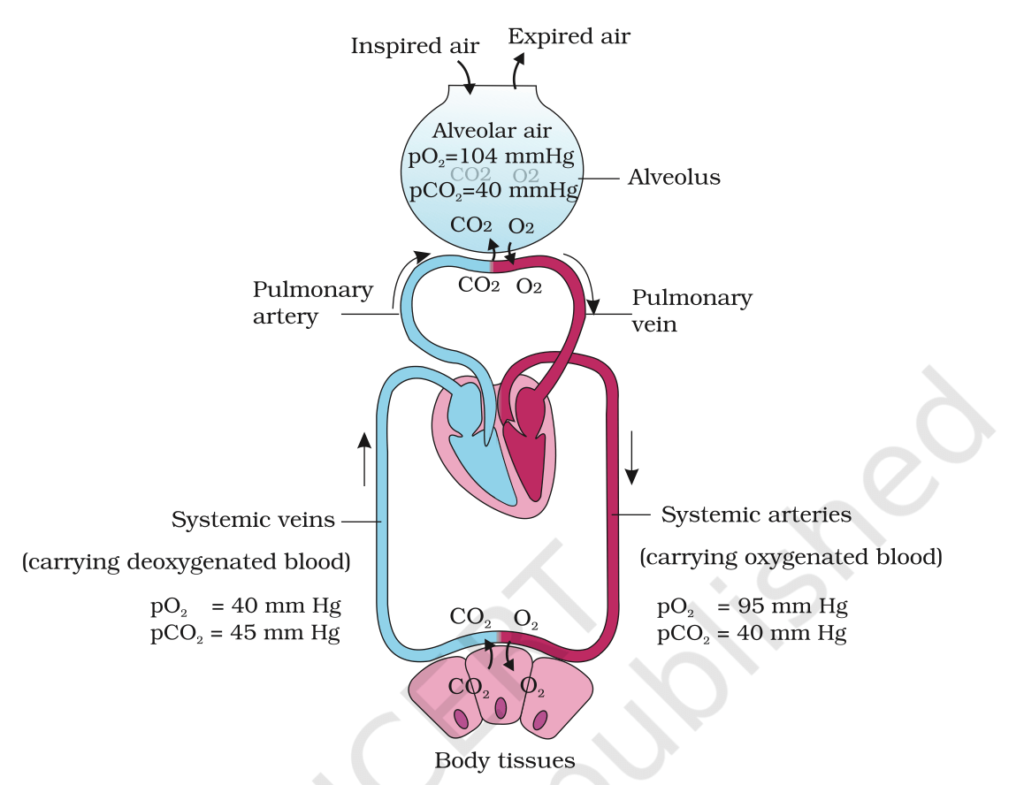
Partial Pressures of Gases:
| Location | O₂ (mm Hg) | CO₂ (mm Hg) |
| Atmospheric Air | 159 | 0.3 |
| Alveoli (Deoxygenated) | 104 | 40 |
| Blood (Oxygenated) | 95 | 40 |
| Tissues | 40 | 45 |
Pressure Gradient: Gases move from higher to lower partial pressure.
- Oxygen diffuses from the alveoli (where its partial pressure is higher) to the blood (where its partial pressure is lower).
- Similarly, carbon dioxide diffuses from the tissues (where its partial pressure is higher) to the blood and then to the alveoli (where its partial pressure is lower)
Oxygen (O₂):
- Alveoli (↑pO₂) → Blood → Tissues (↓pO₂)
Carbon Dioxide (CO₂):
- Tissues (↑pCO₂) → Blood → Alveoli (↓pCO₂)
CO₂ vs. O₂ Diffusion
- CO₂ Solubility: 20-25× higher than O₂ → faster diffusion despite lower gradient.
Transport of Gases
Transport of Oxygen (O₂):
Oxygen is transported in the blood primarily by hemoglobin in red blood cells, with a small amount dissolved directly in plasma.
- Hemoglobin as Oxygen Carrier
- Structure: 4 polypeptide chains, each with a heme group (Fe²⁺ atom )→ binds 1 O₂ molecule.
- Reversible Binding → O₂ binds in lungs, released in tissues.
- Oxygen Hemoglobin Dissociation (Sigmoid Curve)
- High pO₂ (Lungs): O₂ binds to hemoglobin → Forms oxyhemoglobin.
- Low pO₂ (Tissues): O₂ released from oxyhemoglobin.
- Influenced by: ↑pCO₂, ↓pH, ↑temperature → ↓O₂ affinity (Bohr Effect).
Transport of Carbon Dioxide (CO₂):
- As Carbaminohemoglobin (20-25%):
- CO₂ + Hemoglobin (Hb): Forms carbaminohemoglobin.
- Haldane Effect:
- O₂ binding to Hb → ↓CO₂ binding.
- O₂ release → ↑CO₂ binding.
- As Bicarbonate Ion (70%):
- Tissues (High CO₂):
- CO₂ + H₂O → carbonic acid H₂CO₃ → bicarbonate ions (HCO₃⁻) and hydrogen ions (H⁺). (via carbonic anhydrase).
- Chloride Shift: HCO₃⁻ exits RBC, Cl⁻ enters.
- Lungs (Low CO₂):
- HCO₃⁻ + H⁺ → H₂CO₃ → CO₂ + H₂O → CO₂ expelled during expiration.
- Tissues (High CO₂):
- Dissolved in Plasma (5-7%):
- A small amount of CO₂ dissolves directly in the plasma and is transported in this form.
| Mode of Transport | % | Details |
| Dissolved in Plasma | 5-7% | CO₂ directly dissolves in blood plasma. |
| Carbaminohemoglobin | 20-25% | CO₂ binds to hemoglobin (amino groups), forming carbaminohemoglobin (favored by deoxygenated hemoglobin). |
| As Bicarbonate Ions (HCO₃⁻) | 70% | CO₂ is converted into bicarbonate ions through the carbonic anhydrase reaction. |
Regulation of Breathing
Breathing is controlled to ensure the body gets enough oxygen and removes carbon dioxide.
- Brain Control:
- The brainstem (medulla and pons) controls breathing:
- Medulla: Sets the basic breathing rhythm and adjusts for normal or heavy breathing (e.g., during exercise).
- Pons: Prevents lungs from overfilling by controlling the length of breaths.
- The brainstem (medulla and pons) controls breathing:
- Chemical Signals:
- Sensors in the brain and blood detect levels of oxygen, carbon dioxide, and acidity:
- High CO₂ or low oxygen signals the brain to breathe faster or deeper.
- Sensors in the brain and blood detect levels of oxygen, carbon dioxide, and acidity:
- Reflexes:
- Stretch Reflex: Stops lungs from over-expanding.
- Irritant Reflex: Triggers coughing or sneezing to clear airways.
Integration of Respiratory and Circulatory Systems
The respiratory and circulatory systems work together to ensure the effective exchange of gases:
- Pulmonary Circulation: Blood carries CO₂ to the lungs to be exhaled and absorbs O₂ for the body.
- Systemic Circulation: Oxygenated blood from the lungs is delivered to tissues, and CO₂ from tissues is carried back to the lungs for removal.
Disorders of the Respiratory System
1. Asthma
- Description: Chronic condition → Inflammation & narrowing of airways → Wheezing, breathlessness, chest tightness, cough.
- Causes: Allergens, infections, pollution, physical exertion.
- Pathophysiology:
- Bronchi/bronchioles inflamed & constricted → Reduced airflow → Difficulty exhaling.
- Management:
- Bronchodilators (relieve airway constriction).
- Anti-inflammatory drugs (e.g., corticosteroids).
- Trigger avoidance.
2. Emphysema
- Description: Chronic disease → Alveolar wall damage → ↓Surface area for gas exchange → Impaired oxygen/CO₂ transfer.
- Causes:
- Smoking (primary cause).
- Long-term pollutant exposure.
- Genetic: Alpha-1 antitrypsin deficiency.
- Pathophysiology:
- ↓Lung elasticity → Air trapping → Barrel chest.
- Difficulty expelling air → Inefficient gas exchange.
- Symptoms:
- Shortness of breath, chronic cough, chest tightness, barrel-shaped chest.
- Management:
- Smoking cessation (essential).
- Bronchodilators, oxygen therapy.
- Pulmonary rehabilitation.
Clinical Significance of Respiratory Mechanisms
- Hypoxia: ↓O₂ in tissues → Detected by peripheral chemoreceptors → ↑Respiratory rate & depth.
- Hypercapnia: ↑CO₂ in blood → Leads to respiratory acidosis (↓pH) → Body compensates by ↑Respiratory rate → Expels CO₂, restores pH.
- Spirometry: Diagnostic test to assess lung function (e.g., asthma, COPD). Measures air volume exchanged during breathing.